The Kidneys Are Stimulated To Produce Renin ________.
Holbox
Mar 14, 2025 · 6 min read
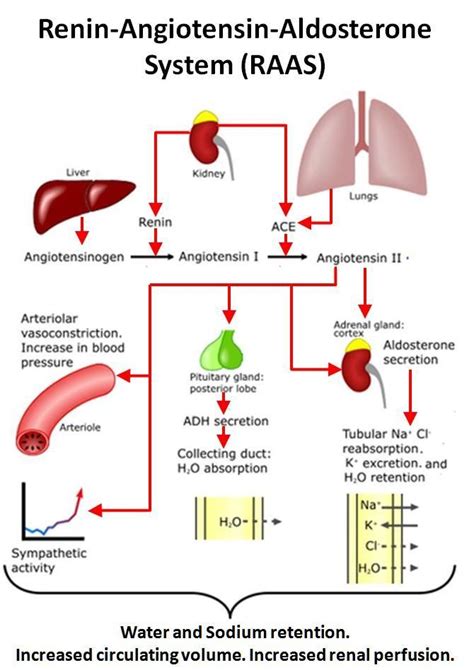
Table of Contents
The Kidneys are Stimulated to Produce Renin: A Deep Dive into Renin-Angiotensin-Aldosterone System (RAAS)
The kidneys, vital organs responsible for filtering waste from the blood, play a crucial role in maintaining blood pressure homeostasis. A key component of this regulation is the production of renin, an enzyme that initiates a cascade of events known as the Renin-Angiotensin-Aldosterone System (RAAS). Understanding the precise stimuli that trigger renin release is fundamental to comprehending blood pressure control and the pathophysiology of hypertension and other related conditions. This article delves into the intricacies of renin release, exploring the various mechanisms and factors involved.
Understanding the Renin-Angiotensin-Aldosterone System (RAAS)
Before we explore the specific stimuli for renin release, let's establish a foundational understanding of the RAAS. This system is a hormonal pathway crucial for regulating blood volume and blood pressure. It's a complex interplay of several hormones and enzymes:
-
Renin: This enzyme, produced by the juxtaglomerular (JG) cells in the kidneys, is the initiating factor. Its release is precisely controlled and responds to specific physiological changes.
-
Angiotensinogen: This inactive protein is produced by the liver and circulates in the blood. Renin cleaves angiotensinogen, converting it to angiotensin I.
-
Angiotensin I: This is an inactive peptide that is further processed by angiotensin-converting enzyme (ACE).
-
Angiotensin-Converting Enzyme (ACE): Primarily located in the lungs, ACE converts angiotensin I to angiotensin II.
-
Angiotensin II: This is the primary active component of the RAAS. It has potent vasoconstricting effects, raising blood pressure directly. It also stimulates aldosterone release from the adrenal glands.
-
Aldosterone: This hormone, produced by the adrenal cortex, acts on the kidneys to increase sodium and water reabsorption, further increasing blood volume and blood pressure.
This intricate system works in a feedback loop, ensuring that blood pressure remains within a tightly controlled range. Dysregulation of the RAAS can lead to hypertension, heart failure, and other cardiovascular complications.
Key Stimuli for Renin Release: A Detailed Examination
The release of renin from the JG cells is a tightly regulated process, responding to several important stimuli. These stimuli can be broadly categorized as:
1. Decreased Renal Perfusion Pressure (RPP): The Primary Stimulus
The most significant stimulus for renin release is a reduction in renal perfusion pressure (RPP). This refers to the blood pressure within the renal arteries, the vessels supplying blood to the kidneys. When RPP decreases, the JG cells detect this change through specialized baroreceptors within their cell membranes. This reduction in pressure triggers a series of intracellular events leading to renin release. This mechanism is crucial for maintaining blood pressure during periods of hypovolemia (low blood volume) or hypotension (low blood pressure).
2. Sympathetic Nervous System Activation: A Powerful Influencer
The sympathetic nervous system (SNS) plays a significant role in regulating blood pressure. During periods of stress or decreased blood pressure, the SNS is activated, releasing norepinephrine. Norepinephrine acts on beta-1 adrenergic receptors located on the JG cells, stimulating renin release. This provides a rapid response mechanism to increase blood pressure in emergency situations.
3. Decreased Sodium Delivery to the Distal Tubule: The Macula Densa's Role
The macula densa, a specialized group of cells located in the distal convoluted tubule (DCT) of the nephron, plays a crucial role in regulating renin release. These cells sense the concentration of sodium chloride in the tubular fluid. When sodium delivery to the DCT decreases, the macula densa signals the JG cells to increase renin release. This feedback mechanism ensures that sodium levels and, consequently, blood volume, are maintained within the normal range. The mechanism by which the macula densa communicates with the JG cells is complex and involves paracrine signaling molecules.
4. Other Factors Influencing Renin Secretion: A Holistic Perspective
While the above three stimuli are the primary triggers, several other factors can modulate renin release:
-
Atrial Natriuretic Peptide (ANP): Released from the atria of the heart in response to increased blood volume, ANP inhibits renin release, acting as a counter-regulatory mechanism.
-
Prostaglandins: These lipid mediators can influence renin release, with some promoting and others inhibiting its secretion. The overall effect depends on the specific prostaglandin and the prevailing physiological conditions.
-
Angiotensin II: While angiotensin II stimulates aldosterone release, it also exerts a negative feedback mechanism, inhibiting further renin release once blood pressure has returned to normal. This prevents excessive activation of the RAAS.
-
Potassium: Increased extracellular potassium concentration can stimulate renin release.
-
Calcium: Changes in extracellular calcium levels can also modulate renin secretion, though the precise mechanisms are still being investigated.
Clinical Implications of Renin Regulation
Understanding the intricacies of renin release is crucial for the diagnosis and management of various clinical conditions. Dysregulation of the RAAS is implicated in several diseases, including:
-
Hypertension: Overactivation of the RAAS contributes to elevated blood pressure. ACE inhibitors and angiotensin receptor blockers (ARBs) are commonly used to inhibit the RAAS and lower blood pressure.
-
Heart Failure: In heart failure, the kidneys often compensate by activating the RAAS, further increasing cardiac workload and worsening the condition. RAAS inhibitors are frequently employed to manage heart failure symptoms.
-
Chronic Kidney Disease (CKD): CKD often leads to reduced renal perfusion pressure, stimulating excessive renin release. This can further exacerbate kidney damage. Careful management of the RAAS is essential in CKD.
-
Pre-eclampsia: This pregnancy-related condition is characterized by hypertension and proteinuria, often linked to dysregulation of the RAAS.
Conclusion: A Complex System with Far-Reaching Effects
The kidneys are stimulated to produce renin in response to a complex interplay of factors, primarily aimed at maintaining blood pressure and fluid homeostasis. Understanding the precise mechanisms involved – decreased renal perfusion pressure, sympathetic nervous system activation, and decreased sodium delivery to the distal tubule – is vital for comprehending the physiology of blood pressure regulation and the pathophysiology of several cardiovascular diseases. The interplay of various hormonal and neural factors involved underscores the complexity and precision of this vital system. Further research continues to refine our understanding of the RAAS, leading to better diagnostics and therapeutics for a wide range of conditions. The intricate balance of these stimuli highlights the remarkable adaptive capabilities of the human body and the critical role of the kidneys in maintaining overall health.
Future Research Directions and Unanswered Questions
While significant progress has been made in understanding renin release, several areas remain open to further investigation:
-
Clarifying the precise intracellular signaling pathways: The exact mechanisms by which reduced renal perfusion pressure, sympathetic activation, and macula densa signaling trigger renin release require further elucidation. Detailed studies at the molecular and cellular level are needed.
-
Investigating the role of other potential regulators: While several factors influencing renin secretion are known, the possibility of other, yet undiscovered regulators remains. High-throughput screening techniques and advanced genomic approaches could identify novel players in the RAAS.
-
Developing more sophisticated therapeutic targets: A deeper understanding of the RAAS could lead to the development of more targeted and effective therapies for hypertension, heart failure, and other related conditions, minimizing side effects and maximizing therapeutic efficacy.
-
Personalized medicine approaches: Individual variability in RAAS activity exists. Investigating genetic and environmental factors influencing this variability could lead to personalized treatment strategies, tailoring therapies to individual needs and responses.
-
Exploring the role of the RAAS in other physiological processes: While primarily associated with blood pressure regulation, the RAAS may have broader roles in other physiological processes, such as inflammation and tissue repair. Further investigation is needed to fully elucidate these potential roles.
The continuing exploration of the mechanisms regulating renin production holds significant promise for advancing our understanding of human physiology and improving the treatment of a wide array of prevalent health conditions. The field of RAAS research remains dynamic and vibrant, with ongoing discoveries continually refining our understanding of this vital system.
Latest Posts
Latest Posts
-
Which Of The Following Disorders Involves The Vertebrae
Mar 14, 2025
-
How Does The Full Path Attribution Model Calculate Credit
Mar 14, 2025
-
The Allowance Method Is Required By
Mar 14, 2025
-
A Circuit Is Constructed With 5 Capacitors And A Battery
Mar 14, 2025
-
Identify The Stages Of Meiosis On The Diagram
Mar 14, 2025
Related Post
Thank you for visiting our website which covers about The Kidneys Are Stimulated To Produce Renin ________. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
