Peripartum Onset Depression Is A Kind Of Depression ________.
Holbox
Mar 14, 2025 · 6 min read
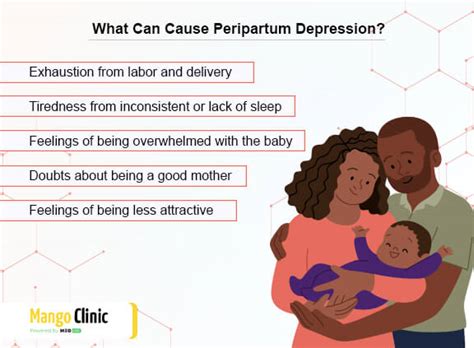
Table of Contents
Peripartum Onset Depression is a Kind of Depression: Understanding the Unique Challenges
Peripartum onset depression is a kind of depression that specifically occurs during pregnancy or within the first year after childbirth. It's crucial to understand that this isn't just "baby blues"—a common experience of mood swings and tearfulness in the postpartum period—but a serious mental health condition requiring professional help. While sharing similarities with other forms of depression, peripartum onset depression possesses unique characteristics, challenges, and implications for both the mother and her baby.
Understanding the Scope of Peripartum Depression
Peripartum depression is more than just feeling sad or overwhelmed. It’s a clinical condition characterized by persistent sadness, despair, anxiety, and a loss of interest in activities once enjoyed. The symptoms can range from mild to severe, significantly impacting a mother's ability to function and care for herself and her baby. It’s essential to dispel the stigma surrounding postpartum depression and recognize that it's a treatable illness, not a personal failing.
Key Symptoms of Peripartum Onset Depression:
- Persistent sadness or low mood: This goes beyond the occasional sadness experienced by new mothers. It's a pervasive feeling of hopelessness and despair.
- Loss of interest or pleasure: Activities that once brought joy now feel meaningless or unappealing.
- Changes in appetite or sleep: This can manifest as either significant weight loss or gain, or insomnia or hypersomnia (excessive sleeping).
- Fatigue or loss of energy: Feeling constantly exhausted, even after adequate rest.
- Feelings of worthlessness or excessive guilt: Intense self-criticism and feelings of inadequacy, often focused on perceived failings as a mother.
- Difficulty concentrating or making decisions: Struggling to focus on tasks, even simple ones.
- Recurrent thoughts of death or suicide: This is a serious symptom and requires immediate professional attention.
- Anxiety: Excessive worry, nervousness, or panic attacks.
- Irritability: Increased anger, frustration, or short temper.
- Physical symptoms: Headaches, stomachaches, muscle tension, and other somatic complaints.
It's important to note that not all women will experience all of these symptoms, and the severity can vary greatly. However, the presence of several of these symptoms for a prolonged period (typically two weeks or more) warrants seeking professional help.
Differentiating Peripartum Depression from Baby Blues and Postpartum Psychosis
While peripartum onset depression shares some superficial similarities with other postpartum conditions, it's crucial to understand the distinctions:
Baby Blues:
The baby blues are characterized by mood swings, tearfulness, anxiety, and irritability. These symptoms typically begin within two to three days after childbirth and usually resolve within two weeks. They are considered a normal hormonal adjustment and do not require medical intervention, although support from family and friends can be helpful.
Postpartum Psychosis:
Postpartum psychosis is a rare but serious mental illness that requires immediate medical attention. It involves a break from reality, characterized by hallucinations, delusions, disorganized thinking, and extreme mood swings. It can be life-threatening for both the mother and the baby and necessitates hospitalization and treatment.
Risk Factors for Peripartum Onset Depression:
Several factors can increase a woman's risk of developing peripartum onset depression. These include:
- History of depression or anxiety: Women with a prior history of mood disorders are at a significantly higher risk.
- Family history of depression: A genetic predisposition can increase vulnerability.
- Stressful life events: Major life changes, such as relationship problems, financial difficulties, or job loss, can exacerbate the risk.
- Lack of social support: Insufficient support from partners, family, or friends can increase isolation and vulnerability.
- Unplanned pregnancy: Feeling unprepared or overwhelmed by the pregnancy can contribute to depression.
- Preeclampsia or gestational diabetes: Medical complications during pregnancy can heighten the risk.
- Previous history of traumatic events: Past trauma can significantly impact mental health during the postpartum period.
- Complications during delivery: Difficult or traumatic births can increase vulnerability.
- Breastfeeding difficulties: Challenges with breastfeeding can add to stress and contribute to depression.
The Impact of Peripartum Depression on Mothers and Babies
Peripartum onset depression has far-reaching consequences for both the mother and her child. Untreated depression can lead to:
For Mothers:
- Impaired ability to care for themselves and their babies: Difficulty with basic self-care, neglecting personal hygiene, and struggling to meet the baby's needs.
- Relationship difficulties: Strain on marital or partner relationships due to emotional distance and conflict.
- Increased risk of substance abuse: Using drugs or alcohol as a coping mechanism.
- Reduced quality of life: Experiencing significant distress and diminished enjoyment of life.
- Increased risk of future episodes of depression: Untreated peripartum depression can increase the likelihood of recurrence.
- Increased risk of suicide: Suicidal thoughts and attempts are a serious concern.
For Babies:
- Delayed development: Difficulties with social, emotional, and cognitive development.
- Attachment problems: Difficulties forming a secure attachment with the mother.
- Behavioral problems: Increased irritability, anxiety, and difficulty regulating emotions.
- Sleep disturbances: Difficulties with sleep patterns and regularity.
- Increased risk of future mental health problems: Children of mothers with peripartum depression are at a higher risk of developing mental health issues themselves.
Seeking Help and Treatment for Peripartum Onset Depression
It's crucial to emphasize that peripartum onset depression is treatable. Seeking professional help is essential, and there are several effective treatment options:
- Therapy: Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT) are commonly used to address negative thought patterns and improve coping skills.
- Medication: Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can be effective in managing symptoms. It's important to discuss medication options with a healthcare professional, considering the potential impact on breastfeeding.
- Support groups: Connecting with other mothers experiencing similar challenges can provide valuable support and reduce feelings of isolation.
- Lifestyle changes: Regular exercise, healthy diet, adequate sleep, and stress-reduction techniques can be helpful in managing symptoms.
It's crucial to seek help early. The sooner treatment begins, the better the chances of recovery and minimizing the long-term impact on both the mother and her child. Women should not hesitate to reach out to their healthcare provider, therapist, or other support systems if they are experiencing symptoms of peripartum onset depression.
The Importance of Early Intervention and Prevention
Early intervention and preventative measures are critical in addressing peripartum onset depression. This includes:
- Prenatal care: Regular check-ups with an obstetrician or midwife provide opportunities to screen for depression and address any concerns.
- Screening tools: Using validated screening tools to identify women at risk.
- Education and awareness: Educating expectant and new mothers about the symptoms, risks, and treatment options for peripartum depression.
- Support systems: Encouraging strong social support networks for mothers, involving family, friends, and community resources.
- Access to mental health services: Ensuring readily available and affordable access to mental healthcare for women in the peripartum period.
Conclusion: A Holistic Approach to Peripartum Depression
Peripartum onset depression is a serious mental health condition with significant consequences for mothers and their babies. It's vital to understand that it’s a treatable illness, not a personal failing. A holistic approach that combines therapeutic interventions, medication when necessary, supportive relationships, and lifestyle modifications is often the most effective strategy for managing and overcoming peripartum depression. Early intervention, prevention efforts, and the reduction of stigma are crucial in improving the lives of mothers and their children. Remember, seeking help is a sign of strength, not weakness, and it's a crucial step towards recovery and well-being. It is essential for healthcare providers, family members, and society as a whole to offer support and understanding to mothers experiencing this challenging period.
Latest Posts
Latest Posts
-
Locate The Centroid Y Of The Area
Mar 14, 2025
-
If Intermediate Goods And Services Were Included In Gdp
Mar 14, 2025
-
After You Return A Check To A Customer
Mar 14, 2025
-
The Internet Is A Collection Of
Mar 14, 2025
-
Consider The Following Reaction At Equilibrium
Mar 14, 2025
Related Post
Thank you for visiting our website which covers about Peripartum Onset Depression Is A Kind Of Depression ________. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
