Part B Practice Interpreting Electrocardiograms Answers
Holbox
Mar 23, 2025 · 7 min read
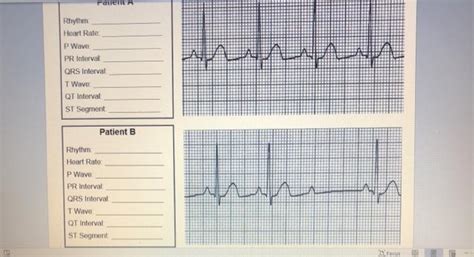
Table of Contents
- Part B Practice Interpreting Electrocardiograms Answers
- Table of Contents
- Part B Practice Interpreting Electrocardiograms: Answers and Comprehensive Guide
- Understanding the Basics: Before We Tackle Part B
- 1. Heart Rate:
- 2. Rhythm:
- 3. P Waves:
- 4. QRS Complexes:
- 5. ST Segments and T Waves:
- Part B Practice ECG Interpretations: Sample Questions and Answers
- Beyond the Basics: Advanced ECG Interpretation Considerations
- Improving Your ECG Interpretation Skills
- Conclusion
- Latest Posts
- Latest Posts
- Related Post
Part B Practice Interpreting Electrocardiograms: Answers and Comprehensive Guide
Interpreting electrocardiograms (ECGs) is a crucial skill for healthcare professionals. This comprehensive guide provides answers and detailed explanations for Part B practice ECG interpretations, focusing on identifying key features and understanding their clinical significance. We will cover various ECG abnormalities, including arrhythmias, ischemia, and infarction. Remember, this guide serves as an educational tool; always consult with a qualified healthcare professional for any medical concerns.
Understanding the Basics: Before We Tackle Part B
Before diving into the answers for Part B practice ECG interpretations, let's refresh some fundamental ECG concepts. The ECG represents the electrical activity of the heart, providing insights into its rhythm, rate, and conduction pathways. Key elements to analyze include:
1. Heart Rate:
Determining the heart rate is paramount. Common methods include:
- Counting R-R intervals: Measure the distance between two consecutive R waves and extrapolate to a 6-second strip (30 large squares).
- Using a quick estimation method: Count the number of large squares between two consecutive R waves and divide 300 by that number.
2. Rhythm:
Analyzing the regularity of R-R intervals helps identify the rhythm. Is it regular, irregularly irregular, or regularly irregular? A regular rhythm suggests a consistent heartbeat, while irregularities may indicate underlying abnormalities.
3. P Waves:
P waves represent atrial depolarization. Their morphology (shape and size), presence, and relationship to QRS complexes are crucial. Absent P waves or abnormal P wave morphology can signal atrial fibrillation, atrial flutter, or other atrial issues.
4. QRS Complexes:
QRS complexes represent ventricular depolarization. Their duration and morphology provide information about ventricular activation. Wide QRS complexes (>0.12 seconds) often indicate conduction delays or ventricular arrhythmias.
5. ST Segments and T Waves:
The ST segment and T wave reflect ventricular repolarization. ST segment elevation or depression, and T wave inversions, are often indicative of myocardial ischemia or infarction.
Part B Practice ECG Interpretations: Sample Questions and Answers
Let's delve into specific ECG examples and their interpretations. Remember, these examples are for educational purposes and shouldn't substitute professional medical advice.
Example 1: Sinus Tachycardia
ECG Characteristics: Regular rhythm, heart rate >100 bpm, normal P waves preceding each QRS complex, normal QRS duration.
Interpretation: Sinus tachycardia. This indicates a rapid heart rate originating from the sinoatrial (SA) node. Possible causes include exercise, stress, fever, dehydration, and certain medications.
Example 2: Atrial Fibrillation
ECG Characteristics: Irregularly irregular rhythm, absence of discernible P waves, narrow QRS complexes, varying R-R intervals.
Interpretation: Atrial fibrillation. This is a common arrhythmia characterized by chaotic atrial activity. Clinical implications can range from asymptomatic to serious, potentially leading to stroke, heart failure, or other complications.
Example 3: Atrial Flutter
ECG Characteristics: Regularly irregular rhythm, characteristic "sawtooth" pattern of flutter waves (F waves) replacing P waves, narrow QRS complexes.
Interpretation: Atrial flutter. This arrhythmia involves rapid atrial activity, often with a flutter rate of 250-350 bpm. The ventricular rate depends on the atrioventricular (AV) node conduction.
Example 4: Ventricular Tachycardia
ECG Characteristics: Rapid heart rate (>100 bpm), wide QRS complexes (>0.12 seconds), often bizarre QRS morphology, absence of P waves.
Interpretation: Ventricular tachycardia. This is a serious arrhythmia where the ventricles beat rapidly and irregularly. It can lead to hemodynamic compromise and requires immediate medical attention.
Example 5: Left Bundle Branch Block (LBBB)
ECG Characteristics: Wide QRS complexes (>0.12 seconds), notched or slurred R waves in the left precordial leads (V5, V6), ST segment and T wave changes often opposite in direction to the main QRS deflection.
Interpretation: Left bundle branch block. This represents a delay or block in the left bundle branch conduction pathway. It can be benign or associated with underlying heart disease.
Example 6: Right Bundle Branch Block (RBBB)
ECG Characteristics: Wide QRS complexes (>0.12 seconds), RSR' pattern (rabbit ears) in the right precordial leads (V1, V2), slurred S waves in the left precordial leads.
Interpretation: Right bundle branch block. Similar to LBBB, RBBB represents a delay or block in the right bundle branch conduction pathway. It can also be benign or associated with underlying cardiac disease.
Example 7: ST-Segment Elevation Myocardial Infarction (STEMI)
ECG Characteristics: ST-segment elevation in at least two contiguous leads, often accompanied by reciprocal ST-segment depression in other leads, inverted T waves.
Interpretation: STEMI. This signifies acute myocardial infarction (heart attack) with significant blockage of a coronary artery. It's a time-sensitive emergency requiring immediate intervention.
Example 8: ST-Segment Depression Myocardial Ischemia
ECG Characteristics: ST-segment depression, often accompanied by T wave inversion in multiple leads, indicating myocardial ischemia (reduced blood flow).
Interpretation: Myocardial ischemia. This signifies reduced blood flow to the heart muscle. The ischemia can be stable angina (predictable chest pain with exertion) or unstable angina (new-onset or worsening chest pain).
Example 9: First-Degree Atrioventricular Block
ECG Characteristics: Prolonged PR interval (>0.20 seconds), consistent PR interval throughout the ECG.
Interpretation: First-degree AV block. This represents a delay in the conduction of the electrical impulse from the atria to the ventricles. It is often asymptomatic and may not require treatment.
**Example 10: Second-Degree Atrioventricular Block (Mobitz Type I/Wenckebach) **
ECG Characteristics: Progressive lengthening of the PR interval until a P wave is not followed by a QRS complex, followed by a shorter PR interval then the cycle repeats.
Interpretation: Second-degree AV block (Mobitz type I/Wenckebach). This indicates an intermittent block in AV conduction. The condition is usually benign, but it can be a precursor to more serious AV blocks.
Example 11: Second-Degree Atrioventricular Block (Mobitz Type II)
ECG Characteristics: Consistent PR interval, but some P waves are not conducted to the ventricles; resulting in dropped QRS complexes. The dropped QRS complexes are not preceded by PR interval lengthening.
Interpretation: Second-degree AV block (Mobitz type II). This is a more serious form of AV block compared to Mobitz Type I because it often indicates a more significant impairment in AV node conduction. It requires close monitoring.
Example 12: Third-Degree Atrioventricular Block (Complete Heart Block)
ECG Characteristics: Complete dissociation between atrial and ventricular activity; P waves and QRS complexes are independent of each other; the heart rate is slower.
Interpretation: Third-degree AV block (complete heart block). This is a complete block in the conduction pathway between the atria and ventricles, resulting in the atria and ventricles beating independently. It is a life-threatening condition that often requires a pacemaker.
Beyond the Basics: Advanced ECG Interpretation Considerations
Accurate ECG interpretation requires considering various factors beyond the basic elements discussed above:
-
Patient History: Understanding the patient's medical history (e.g., prior heart conditions, medications, symptoms) is crucial for contextualizing the ECG findings.
-
Clinical Presentation: The patient's symptoms (e.g., chest pain, shortness of breath, palpitations) provide essential information to correlate with the ECG interpretation.
-
Lead Placement: Proper lead placement is essential for accurate ECG interpretation. Incorrect lead placement can lead to misinterpretations.
-
Electrolyte Imbalances: Electrolyte abnormalities (e.g., potassium, magnesium) can significantly affect ECG morphology.
-
Medication Effects: Certain medications can influence the appearance of the ECG.
Improving Your ECG Interpretation Skills
Mastering ECG interpretation requires consistent practice and a structured learning approach. Here are some strategies:
-
Utilize Online Resources: Numerous online resources, including interactive ECG interpretation tools, can enhance your learning.
-
Study ECG Cases: Analyze numerous ECG examples, focusing on identifying key features and correlating them with clinical scenarios.
-
Seek Mentorship: If possible, seek guidance from experienced healthcare professionals who can provide feedback and answer questions.
-
Participate in ECG Workshops: Attending ECG interpretation workshops can provide valuable hands-on experience and insights.
-
Focus on Pattern Recognition: Develop your ability to quickly identify common ECG patterns. With practice, you will recognize patterns associated with specific conditions.
Conclusion
ECG interpretation is a complex but essential skill for healthcare professionals. This guide provides answers to sample Part B practice ECG interpretations, offering explanations of key features and their clinical significance. Remember, accurate ECG interpretation requires a holistic approach, incorporating patient history, clinical presentation, and a thorough understanding of ECG principles. Continuous learning and practice are crucial for improving ECG interpretation skills and ensuring accurate diagnosis and treatment of cardiac conditions. Always prioritize patient safety and seek expert consultation when necessary.
Latest Posts
Latest Posts
-
An Operation Must Hire A Pest Control Operator Who Is
Mar 26, 2025
-
A Financial Advisor Is Cold Calling Leads
Mar 26, 2025
-
The Allowance For Uncollectible Accounts Is A Contra Account To
Mar 26, 2025
-
Rank The Structures In Order Of Decreasing Electrophile Strength
Mar 26, 2025
-
Perfect Competition Is Characterized By All Of The Following Except
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Part B Practice Interpreting Electrocardiograms Answers . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
