What Direct Effect Do Histamines And Leukotrienes Have On Capillaries
Holbox
Mar 14, 2025 · 5 min read
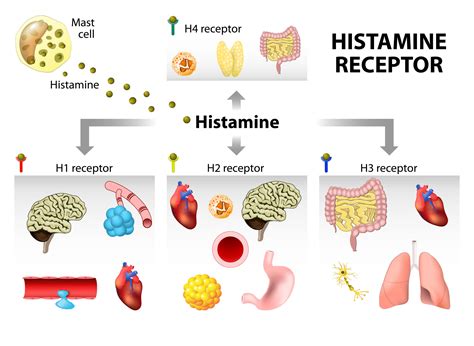
Table of Contents
The Direct Effects of Histamines and Leukotrienes on Capillaries: A Deep Dive into Inflammatory Responses
The intricate network of capillaries, the smallest blood vessels in the body, plays a crucial role in nutrient delivery and waste removal. Their thin walls allow for efficient exchange between blood and surrounding tissues. However, this delicate structure is highly susceptible to inflammatory mediators like histamines and leukotrienes, leading to significant changes in capillary function and contributing to a variety of diseases. This article will delve into the direct effects of histamines and leukotrienes on capillaries, exploring their mechanisms of action and the resulting physiological consequences.
Histamine's Impact on Capillary Function
Histamine, a crucial component of the immune response, is stored in mast cells and basophils. Upon encountering allergens or tissue injury, these cells release histamine, triggering a cascade of events that significantly alter capillary function. Its effects are primarily mediated through the activation of specific histamine receptors, namely H1 and H2 receptors, located on capillary endothelial cells and surrounding smooth muscle.
H1 Receptor-Mediated Effects: Increased Vascular Permeability
The most prominent effect of histamine is the increase in capillary permeability. This occurs primarily through the activation of H1 receptors on endothelial cells. H1 receptor stimulation triggers a series of intracellular signaling pathways that lead to:
-
Contraction of endothelial cells: This creates gaps between adjacent endothelial cells, widening the intercellular junctions. This widening allows the passage of fluid, proteins, and even inflammatory cells from the bloodstream into the surrounding tissues. This process is crucial in the development of edema (swelling) characteristic of allergic reactions and inflammation.
-
Increased expression of adhesion molecules: Histamine stimulation upregulates the expression of adhesion molecules on endothelial cells. These molecules facilitate the binding and extravasation (migration) of leukocytes, such as neutrophils, monocytes, and lymphocytes, from the blood into the inflamed tissue. This influx of inflammatory cells contributes to the amplification of the inflammatory response.
-
Activation of nitric oxide synthase: Histamine can stimulate the production of nitric oxide (NO), a potent vasodilator. NO contributes to the increase in blood flow to the inflamed area, further enhancing the delivery of inflammatory cells and mediators.
H2 Receptor-Mediated Effects: Vasodilation and Increased Blood Flow
While H1 receptors primarily mediate increased vascular permeability, H2 receptors contribute to vasodilation. Activation of H2 receptors on vascular smooth muscle cells leads to relaxation of these cells, resulting in vasodilation and increased blood flow to the affected area. This increased blood flow is essential for delivering immune cells and nutrients to the site of inflammation. However, this dilation can also lead to hypotension (low blood pressure) in severe cases of systemic histamine release.
Leukotrienes' Role in Capillary Alterations
Leukotrienes, a group of lipid mediators derived from arachidonic acid, play a crucial role in inflammation and particularly contribute to the prolonged phase of the inflammatory response. Unlike the rapid action of histamine, leukotrienes exert their effects over a longer period. Their influence on capillaries includes:
Increased Vascular Permeability and Edema Formation
Leukotrienes, especially leukotriene B4 (LTB4), leukotriene C4 (LTC4), leukotriene D4 (LTD4), and leukotriene E4 (LTE4), significantly increase capillary permeability. While the exact mechanisms aren't as fully understood as those of histamine, they involve:
-
Direct effects on endothelial cells: Leukotrienes interact with specific receptors on endothelial cells, triggering intracellular signaling pathways that lead to changes in the cytoskeleton and the widening of intercellular junctions. This, in turn, results in increased permeability.
-
Recruitment of inflammatory cells: LTB4, in particular, is a potent chemoattractant for neutrophils. It attracts neutrophils to the site of inflammation, further enhancing the inflammatory response and contributing to edema formation. These recruited neutrophils contribute to tissue damage through the release of their own inflammatory mediators and reactive oxygen species.
Bronchoconstriction and Airway Inflammation (Indirect effect on Capillaries)
While not a direct effect on capillaries, the bronchoconstriction caused by leukotrienes (LTC4, LTD4, LTE4) can indirectly impact capillary function in the lungs. The constriction of airways can lead to hypoxia (low oxygen levels) in the surrounding tissues, impacting capillary oxygen exchange and potentially leading to further inflammation and tissue damage. This highlights the interconnectedness of inflammatory responses in different organ systems.
Prolonged Inflammatory Response
Leukotrienes contribute to the prolonged phase of inflammation, lasting for hours or even days, unlike the more immediate effects of histamine. This prolonged inflammatory response can cause sustained capillary damage and contribute to chronic inflammatory diseases.
Comparing and Contrasting the Effects of Histamine and Leukotrienes
Both histamine and leukotrienes significantly alter capillary function, contributing to the inflammatory response. However, their actions differ in timing and specific effects:
| Feature | Histamine | Leukotrienes |
|---|---|---|
| Onset | Rapid (seconds to minutes) | Slower (minutes to hours) |
| Duration | Short-lived | Prolonged (hours to days) |
| Primary Effect | Increased vascular permeability, vasodilation | Increased vascular permeability, chemotaxis |
| Receptors | H1, H2 | CysLT1, CysLT2, BLT1, BLT2 |
| Principal Mediators | Increased permeability, vasodilation | Increased permeability, chemotaxis, prolonged inflammation |
Clinical Significance and Therapeutic Implications
Understanding the direct effects of histamine and leukotrienes on capillaries is crucial in managing various inflammatory diseases. Conditions where these mediators play a significant role include:
-
Allergic rhinitis: Characterized by nasal congestion, sneezing, and itching due to increased capillary permeability and vasodilation.
-
Asthma: Leukotrienes contribute significantly to airway inflammation and bronchoconstriction, leading to wheezing and shortness of breath.
-
Atopic dermatitis (Eczema): Characterized by skin inflammation with itching and rashes, resulting from increased capillary permeability and inflammatory cell infiltration.
-
Anaphylaxis: A severe, life-threatening allergic reaction involving widespread vasodilation, increased vascular permeability, and hypotension.
Therapeutic interventions often target the actions of these mediators. Antihistamines block histamine receptors, reducing vascular permeability and vasodilation. Leukotriene inhibitors block the actions of leukotrienes, decreasing inflammation and bronchoconstriction. These treatments aim to restore normal capillary function and alleviate symptoms associated with these inflammatory diseases.
Conclusion
Histamine and leukotrienes are potent inflammatory mediators that exert significant direct effects on capillaries. Histamine rapidly increases capillary permeability and vasodilation primarily via H1 and H2 receptor activation, while leukotrienes contribute to prolonged increases in permeability and chemotaxis, leading to a sustained inflammatory response. Understanding their distinct mechanisms is crucial for developing effective therapies targeting inflammatory conditions characterized by capillary dysfunction. Further research into the intricate interactions of these mediators and their impact on capillary structure and function promises to yield valuable insights for the development of novel therapeutic strategies in the future. The complex interplay between these inflammatory mediators and the delicate balance of capillary function underscores the importance of targeted therapies for managing a wide range of inflammatory diseases.
Latest Posts
Latest Posts
-
A Cutomer Calls Because Her Internet Isnt Working
Mar 15, 2025
-
A Customer At A Table Has A Soy Allergy
Mar 15, 2025
-
A Production Possibilities Frontier Is Bowed Outward When
Mar 15, 2025
-
What Conclusions Can We Draw From Trait Theory
Mar 15, 2025
-
The Internet Is Primarily Funded By
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about What Direct Effect Do Histamines And Leukotrienes Have On Capillaries . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
