Uteroplacental Flow Is Absent At This Intrauterine Pressure
Holbox
Mar 11, 2025 · 7 min read
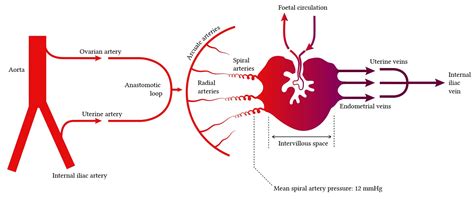
Table of Contents
Uteroplacental Flow is Absent at This Intrauterine Pressure: Understanding the Implications
The statement "uteroplacental flow is absent at this intrauterine pressure" signifies a critical obstetric emergency. It indicates a complete cessation of blood flow between the mother and the fetus via the placenta, a condition with devastating consequences for fetal well-being and survival. This article delves into the underlying causes, diagnostic methods, management strategies, and the crucial role of intrauterine pressure monitoring in understanding and addressing this life-threatening complication.
Understanding Uteroplacental Circulation
Before examining the absence of uteroplacental flow, it's crucial to understand its normal physiology. The uteroplacental circulation is the lifeblood of the developing fetus, providing oxygen, nutrients, and removing waste products. This complex system involves the spiral arteries within the uterine wall, the intervillous space of the placenta, and the fetal circulation. Blood flows from the maternal spiral arteries into the intervillous space, bathing the placental villi rich in fetal capillaries. Here, gas exchange and nutrient transfer occur. The blood then drains back into the maternal venous system. The integrity and efficiency of this system are paramount for fetal health.
Key Components of Healthy Uteroplacental Circulation:
- Adequate Maternal Blood Volume and Pressure: Sufficient blood volume and pressure are essential to perfuse the intervillous space effectively.
- Patent Spiral Arteries: These arteries must be appropriately remodeled during pregnancy to allow for optimal blood flow. Failure of this remodeling can lead to insufficient flow.
- Healthy Placental Structure: The placenta must be structurally intact to facilitate efficient exchange. Placental abruption, infarction, or other abnormalities can compromise flow.
- Normal Fetal Vascular Resistance: High fetal vascular resistance can impede return flow from the placenta.
Causes of Absent Uteroplauterine Flow
The absence of uteroplacental flow at a given intrauterine pressure indicates a severe disruption of this vital system. Several critical factors can contribute to this catastrophic event:
1. Uterine Atony:
Severe uterine atony, or the inability of the uterus to contract effectively, can significantly reduce or completely halt uteroplacental flow. This can occur postpartum, leading to postpartum hemorrhage, where blood loss is substantial, and uteroplacental perfusion is severely compromised.
2. Placental Abruption:
Placental abruption, the premature separation of the placenta from the uterine wall, is a major cause of fetal compromise. This separation interrupts the blood flow, resulting in fetal hypoxia and acidosis. The severity of abruption directly correlates with the extent of placental detachment and resultant disruption to uteroplacental perfusion.
3. Uterine Rupture:
Uterine rupture, a complete or partial tear in the uterine wall, is a life-threatening obstetric emergency. This catastrophic event can severely compromise or completely halt uteroplacental flow, causing immediate fetal distress. It often presents with sudden abdominal pain, fetal heart rate abnormalities, and maternal shock.
4. Amniotic Fluid Embolism:
Amniotic fluid embolism, a rare but devastating complication, involves the entry of amniotic fluid into the maternal circulation. This can cause severe respiratory distress, cardiovascular collapse, and disseminated intravascular coagulation (DIC), which indirectly affects uteroplacental perfusion by reducing blood flow to the uterus.
5. Severe Pre-eclampsia or Eclampsia:
Severe pre-eclampsia or eclampsia can lead to significant vasoconstriction, reducing blood flow to the uterus and placenta. The resulting placental ischemia can compromise uteroplacental flow, leading to fetal growth restriction and other adverse outcomes.
6. Uterine Thromboembolism:
While less common, uterine thromboembolism can obstruct blood flow to sections of the uterus, resulting in localized placental insufficiency. This can contribute to a significant reduction in overall uteroplacental flow, especially if a large vessel is affected.
Diagnostic Approaches
Diagnosing absent uteroplacental flow requires a combination of clinical assessment and advanced imaging techniques:
-
Fetal Heart Rate Monitoring: Continuous fetal heart rate monitoring is crucial. Absent or severely compromised uteroplacental flow will manifest as a non-reassuring fetal heart rate pattern, including bradycardia, tachycardia, late decelerations, and variable decelerations.
-
Ultrasound: Ultrasound examination can assess placental morphology, identify placental abruption or other structural abnormalities, and evaluate amniotic fluid volume. Doppler ultrasound can assess the velocity of blood flow within the uterine arteries and umbilical cord. The absence of flow in Doppler studies strongly suggests compromised or absent uteroplacental perfusion.
-
Intrauterine Pressure Monitoring (IUPM): IUPM, combined with other monitoring techniques, provides crucial information about uterine contractility and its relationship to uteroplacental blood flow. Absent flow in the context of abnormal IUPM readings may indicate uterine atony or other causes of circulatory impairment.
-
Blood Tests: Blood tests may reveal markers of fetal distress, such as acidosis or decreased oxygen saturation. Maternal blood tests can help identify conditions like DIC or other systemic complications.
Management Strategies
The management of absent uteroplacental flow is dictated by the underlying cause and the severity of the condition. Immediate intervention is typically required to save the fetus and mother.
-
Emergency Cesarean Section: If the absence of uteroplacental flow is associated with fetal distress or maternal instability, an emergency cesarean section is the most appropriate intervention. The goal is to deliver the fetus rapidly to minimize the duration of hypoxia.
-
Fluid Resuscitation: If the underlying cause is related to hypovolemia, aggressive intravenous fluid resuscitation may be necessary to restore maternal blood volume and improve uteroplacental perfusion.
-
Blood Transfusion: Significant blood loss may necessitate blood transfusion to correct anemia and maintain maternal hemodynamic stability.
-
Uterine Compression: In cases of uterine atony, bimanual uterine compression or the application of uterotonics (medications that stimulate uterine contractions) may help restore uterine tone and improve blood flow.
-
Treatment of Underlying Conditions: Management also focuses on addressing the specific underlying cause: Placental abruption requires careful monitoring and supportive care. Uterine rupture necessitates immediate surgical repair. Severe pre-eclampsia or eclampsia requires treatment with antihypertensive medications and magnesium sulfate.
Intrauterine Pressure Monitoring (IUPM) and Its Role
Intrauterine pressure monitoring (IUPM) plays a vital role in the diagnosis and management of conditions leading to absent uteroplacental flow. By continuously monitoring uterine contractility, IUPM provides valuable insights into uterine activity and its potential impact on blood flow. Abnormal IUPM readings, such as prolonged high-intensity contractions or hypotonic uterine contractions, can indicate potential disruptions to uteroplacental flow, even before fetal heart rate abnormalities become evident.
IUPM in the Context of Absent Uteroplacental Flow:
-
Identifying Uterine Atony: IUPM can reliably detect uterine atony, a common cause of postpartum hemorrhage and compromised uteroplacental flow. Low intrauterine pressures indicate poor uterine tone, which impairs blood flow through the placenta.
-
Assessing the Impact of Contractions: IUPM can assess whether uterine contractions are adequately perfusing the placenta. Excessive or prolonged contractions may compromise flow, even if the baseline pressure is normal.
Prognosis and Prevention
The prognosis for a fetus with absent uteroplacental flow depends significantly on the underlying cause, the duration of the interruption, and the speed of intervention. Prompt diagnosis and management are crucial for improving fetal outcomes. Unfortunately, in many cases, despite rapid intervention, the outcome may be unfavorable.
Preventive strategies focus on identifying and managing risk factors that can lead to compromised uteroplacental flow. These include:
-
Preconception Counseling: Addressing pre-existing medical conditions, ensuring adequate nutrition, and avoiding smoking and alcohol during pregnancy.
-
Regular Prenatal Care: Close monitoring of maternal health, fetal growth, and placental function throughout the pregnancy.
-
Early Recognition and Management of Pregnancy Complications: Prompt identification and management of conditions such as pre-eclampsia, gestational diabetes, and placental abruption.
Conclusion
The absence of uteroplacental flow represents a critical obstetric emergency with severe consequences for both mother and fetus. Understanding the underlying causes, utilizing advanced diagnostic tools such as IUPM, and implementing prompt management strategies are crucial for improving outcomes. Emphasis on prevention through careful prenatal care and addressing risk factors is equally vital in reducing the incidence of this life-threatening condition. The collaborative effort of an experienced medical team is indispensable for managing this complex obstetric emergency successfully. The implications are severe, and a rapid, coordinated response is essential to improve the chances of survival for both mother and child. Further research is continually needed to improve our understanding of this critical aspect of maternal-fetal physiology and to develop even more effective preventive and treatment strategies.
Latest Posts
Latest Posts
-
Module 11 Assignment Psw Part 2
Mar 11, 2025
-
How Much Unexcused Absenteeism Is Acceptable Per Year
Mar 11, 2025
-
What Must A Server Do To Avoid Over Service
Mar 11, 2025
-
The Last Step Of Proper Manual Dishwashing Procedure Is
Mar 11, 2025
-
What Challenge Does Generative Ai Face With Respect To Data
Mar 11, 2025
Related Post
Thank you for visiting our website which covers about Uteroplacental Flow Is Absent At This Intrauterine Pressure . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
