Match Each Form Of Hypoxia With Its Definition.
Holbox
Apr 02, 2025 · 6 min read
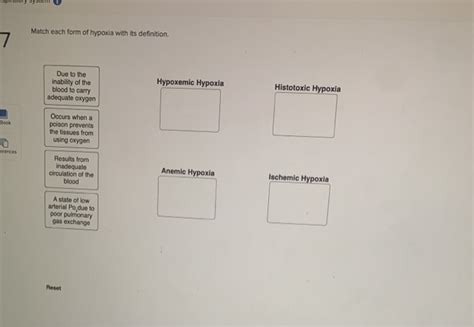
Table of Contents
- Match Each Form Of Hypoxia With Its Definition.
- Table of Contents
- Match Each Form of Hypoxia With Its Definition: A Comprehensive Guide
- Understanding the Basics of Hypoxia
- Categorizing Hypoxia: A Multifaceted Approach
- Causes of Hypoxic Hypoxia:
- Causes of Anemic Hypoxia:
- Causes of Stagnant Hypoxia:
- Causes of Histotoxic Hypoxia:
- Symptoms of Hypoxia: A Wide Spectrum
- Common Symptoms of Hypoxia:
- Diagnosing Hypoxia: A Multi-pronged Approach
- Diagnostic Methods:
- Treatment of Hypoxia: Addressing the Root Cause
- Treatment Strategies:
- Conclusion: A Multifaceted Condition Requiring Precise Diagnosis and Treatment
- Latest Posts
- Latest Posts
- Related Post
Match Each Form of Hypoxia With Its Definition: A Comprehensive Guide
Hypoxia, a condition characterized by insufficient oxygen supply to the body's tissues, presents in various forms, each with unique causes and consequences. Understanding these different types is crucial for medical professionals and anyone interested in human physiology and pathophysiology. This comprehensive guide will meticulously define and differentiate the various forms of hypoxia, exploring their underlying mechanisms and potential implications.
Understanding the Basics of Hypoxia
Before delving into the specific types, it's essential to establish a foundational understanding of hypoxia itself. Hypoxia isn't a disease but rather a condition resulting from a disruption in the body's oxygen delivery system. This disruption can occur at any point along the pathway: from the lungs' intake of oxygen to the utilization of oxygen by the cells. The severity of hypoxia depends on the extent and duration of oxygen deprivation. Mild hypoxia may cause subtle symptoms, while severe hypoxia can lead to organ damage and even death.
Categorizing Hypoxia: A Multifaceted Approach
Hypoxia is broadly categorized based on the underlying cause of oxygen deficiency. These categories are not always mutually exclusive; a patient may experience a combination of different forms simultaneously. We will examine the following classifications:
1. Hypoxic Hypoxia:
This is the most common type of hypoxia, also known as hypoxemic hypoxia. It stems from a reduction in the partial pressure of oxygen (PaO2) in the arterial blood. This means the blood itself isn't carrying enough oxygen.
Causes of Hypoxic Hypoxia:
- High Altitude: At higher altitudes, the atmospheric pressure is lower, resulting in reduced oxygen availability in the inhaled air. This is a classic example of hypoxic hypoxia.
- Hypoventilation: Inadequate breathing, whether due to respiratory muscle weakness, lung disease (like emphysema or pneumonia), or central nervous system depression (e.g., drug overdose), reduces the amount of oxygen entering the lungs.
- Diffusion Impairment: Conditions that affect the diffusion of oxygen across the alveolar-capillary membrane, such as pulmonary fibrosis or pulmonary edema, hinder oxygen uptake into the bloodstream.
- Shunt: A physiological shunt occurs when blood flows through the lungs without participating in gas exchange, bypassing the alveoli where oxygen uptake occurs. Congenital heart defects and certain lung diseases can cause shunting.
- Ventilation-Perfusion Mismatch (V/Q Mismatch): This occurs when ventilation (airflow) and perfusion (blood flow) to the lungs are not properly matched. Areas of the lung might be well-ventilated but poorly perfused, or vice-versa, leading to ineffective oxygen uptake.
2. Anemic Hypoxia:
Anemic hypoxia results from a decreased capacity of the blood to carry oxygen. While the partial pressure of oxygen in the arterial blood might be normal, the blood's oxygen-carrying capacity is reduced.
Causes of Anemic Hypoxia:
- Anemia: This is the most common cause. Anemia is a condition characterized by a deficiency of red blood cells or hemoglobin, the protein in red blood cells that binds to oxygen. Various factors can cause anemia, including iron deficiency, vitamin B12 deficiency, and bone marrow disorders.
- Carbon Monoxide Poisoning: Carbon monoxide (CO) has a much higher affinity for hemoglobin than oxygen. When CO binds to hemoglobin, it prevents oxygen from binding, effectively reducing the blood's oxygen-carrying capacity.
- Methemoglobinemia: This rare condition involves the oxidation of ferrous iron (Fe2+) in hemoglobin to ferric iron (Fe3+), forming methemoglobin, which cannot bind to oxygen.
3. Stagnant Hypoxia:
Also known as ischemic hypoxia, stagnant hypoxia occurs when blood flow to the tissues is reduced or impaired, leading to inadequate oxygen delivery despite normal oxygen content in the arterial blood.
Causes of Stagnant Hypoxia:
- Heart Failure: A weakened heart cannot pump enough blood to meet the body's oxygen demands, resulting in reduced blood flow to the tissues.
- Shock: Shock is a life-threatening condition involving inadequate blood flow to vital organs, often caused by severe injury, infection, or blood loss.
- Thrombosis (Blood Clot): A blood clot can obstruct blood vessels, reducing or completely stopping blood flow to the affected area.
- Edema (Fluid Buildup): Excessive fluid buildup in tissues can compress blood vessels and hinder blood flow.
- Peripheral Vascular Disease (PVD): Conditions like atherosclerosis, narrowing the arteries, can restrict blood flow to the extremities.
4. Histotoxic Hypoxia:
Histotoxic hypoxia occurs when the tissues' ability to utilize oxygen is impaired, even if adequate oxygen is delivered to them. The problem lies not in the delivery of oxygen but in the cells' inability to use it effectively.
Causes of Histotoxic Hypoxia:
- Cyanide Poisoning: Cyanide inhibits cytochrome c oxidase, a crucial enzyme in the electron transport chain, preventing the cells from utilizing oxygen for energy production.
- Certain Drugs and Toxins: Some drugs and toxins can interfere with cellular respiration, impairing oxygen utilization.
- Metabolic Disorders: Some metabolic disorders can disrupt cellular processes involved in oxygen utilization.
Symptoms of Hypoxia: A Wide Spectrum
The symptoms of hypoxia vary greatly depending on the severity and the affected tissues. Mild hypoxia might cause subtle symptoms, while severe hypoxia can lead to life-threatening complications.
Common Symptoms of Hypoxia:
- Shortness of breath (dyspnea): This is a hallmark symptom, especially in hypoxic hypoxia.
- Rapid heart rate (tachycardia): The heart attempts to compensate for reduced oxygen delivery by increasing its pumping rate.
- Increased respiratory rate (tachypnea): The respiratory system tries to increase oxygen intake.
- Cyanosis (bluish discoloration of the skin and mucous membranes): This occurs due to the presence of deoxygenated hemoglobin in the blood. However, it's important to note that cyanosis is not always present, and its absence doesn't rule out hypoxia.
- Headache: Hypoxia can affect the brain, leading to headaches.
- Dizziness and lightheadedness: These are common neurological manifestations.
- Confusion and disorientation: Severe hypoxia can impair cognitive function.
- Fatigue and weakness: Reduced oxygen delivery affects muscle function.
- In severe cases: loss of consciousness, seizures, coma, and even death can occur.
Diagnosing Hypoxia: A Multi-pronged Approach
Diagnosing hypoxia involves a combination of clinical evaluation, physical examination, and laboratory tests.
Diagnostic Methods:
- Pulse oximetry: This non-invasive method measures the oxygen saturation (SpO2) of arterial blood.
- Arterial blood gas (ABG) analysis: This provides precise measurements of PaO2, PaCO2 (partial pressure of carbon dioxide), pH, and bicarbonate levels.
- Complete blood count (CBC): This helps assess for anemia, a key factor in anemic hypoxia.
- Chest X-ray: This can reveal underlying lung conditions that contribute to hypoxic hypoxia.
- Echocardiogram: This can evaluate heart function and identify conditions that might lead to stagnant hypoxia.
Treatment of Hypoxia: Addressing the Root Cause
Treatment of hypoxia depends entirely on the underlying cause. The goal is to restore adequate oxygen delivery to the tissues.
Treatment Strategies:
- Supplemental oxygen: This is the cornerstone of treatment for most forms of hypoxia, delivered via nasal cannula, face mask, or other devices.
- Treatment of underlying conditions: Addressing the root cause of hypoxia, whether it's anemia, heart failure, or lung disease, is essential for long-term management.
- Mechanical ventilation: In severe cases, mechanical ventilation might be necessary to support breathing.
- Blood transfusion: In cases of severe anemia, blood transfusion may be required to increase oxygen-carrying capacity.
- Treatment of poisoning: In cases of carbon monoxide poisoning or cyanide poisoning, specific antidotes are administered.
Conclusion: A Multifaceted Condition Requiring Precise Diagnosis and Treatment
Hypoxia is a complex condition with diverse causes and manifestations. Differentiating between the various forms of hypoxia – hypoxic, anemic, stagnant, and histotoxic – is crucial for accurate diagnosis and effective treatment. Understanding the underlying mechanisms of each type allows healthcare professionals to tailor interventions to restore adequate oxygen delivery and prevent potentially life-threatening complications. Early recognition and prompt management of hypoxia are vital to ensure optimal patient outcomes. This comprehensive guide provides a strong foundation for understanding this critical aspect of human physiology and pathology.
Latest Posts
Latest Posts
-
Released 200 Kg Of In The Water Supplu
Apr 05, 2025
-
Complete The Missing Parts Of The Table On Diabetes Mellitus
Apr 05, 2025
-
Art Labeling Activity Blood Flow Through The Kidney
Apr 05, 2025
-
Rank The Indicated Protons In Decreasing Order Of Acidity
Apr 05, 2025
-
The Drawing Shows A Hydraulic Chamber With A Spring
Apr 05, 2025
Related Post
Thank you for visiting our website which covers about Match Each Form Of Hypoxia With Its Definition. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
