Staphylococcus Aureus Produces A Of The Epidermis And Dermis.
Holbox
Mar 16, 2025 · 6 min read
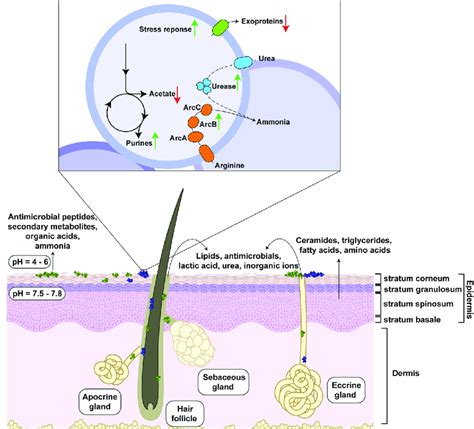
Table of Contents
Staphylococcus Aureus: A Deep Dive into its Impact on the Epidermis and Dermis
Staphylococcus aureus (S. aureus), a ubiquitous bacterium residing on human skin and in the nasal passages, is a significant human pathogen capable of causing a wide spectrum of infections, from mild skin irritations to life-threatening systemic diseases. Its ability to colonize and infect the epidermis and dermis, the two main layers of the skin, is largely dependent on its arsenal of virulence factors. This article will delve into the intricate mechanisms by which S. aureus interacts with the epidermis and dermis, leading to a variety of skin and soft tissue infections (SSTIs).
Understanding the Skin's Defenses
Before exploring S. aureus's pathogenic mechanisms, it's crucial to understand the skin's inherent defense mechanisms. The skin acts as a formidable physical barrier, preventing the entry of pathogens. This barrier comprises:
The Epidermis: The Outermost Shield
The epidermis, the outermost layer, is composed of stratified squamous epithelium, providing a tough, waterproof barrier. Keratinocytes, the predominant cells, produce keratin, a protein contributing to the skin's strength and impermeability. Furthermore, the epidermis harbors Langerhans cells, a type of dendritic cell crucial for initiating immune responses against invading pathogens.
The Dermis: A Deeper Defense
Beneath the epidermis lies the dermis, a thicker layer containing connective tissue, blood vessels, nerves, and hair follicles. The dermis houses fibroblasts, responsible for producing collagen and elastin, providing structural support and elasticity to the skin. Additionally, the dermis contains immune cells, including mast cells and macrophages, which play vital roles in combating infection. The presence of these immune cells and the structural integrity of the dermis contribute significantly to the skin's overall defense against S. aureus.
Staphylococcus Aureus Virulence Factors: Breaching the Skin's Defenses
S. aureus's ability to cause infection hinges on a complex interplay of virulence factors that allow it to:
-
Adhere to the skin: Several adhesins, including fibronectin-binding proteins (FnBPs), clumping factors (ClfA and ClfB), and collagen-binding proteins, mediate S. aureus's attachment to the epidermis and dermis. These adhesins bind to specific host extracellular matrix proteins, enabling the bacteria to firmly colonize the skin surface.
-
Invade the skin: Once adhered, S. aureus employs various strategies to breach the skin barrier. Enzymes such as hyaluronidase, which degrades hyaluronic acid (a component of the extracellular matrix), and lipases, which break down lipids, facilitate bacterial penetration into the deeper skin layers. Furthermore, some S. aureus strains produce toxins that directly damage skin cells, contributing to tissue destruction and facilitating invasion.
-
Evade the immune system: S. aureus possesses a range of mechanisms to evade the host immune response. Protein A binds to the Fc region of antibodies, preventing their opsonization and phagocytosis. Capsules interfere with complement activation and phagocytosis. Furthermore, S. aureus can produce superantigens, such as toxic shock syndrome toxin-1 (TSST-1), which overstimulate the immune system, potentially leading to systemic effects.
-
Spread through the skin: After invasion, S. aureus can spread through the dermis, utilizing its ability to degrade extracellular matrix components and utilizing host cells for dissemination. This spread can result in localized or widespread infections, depending on the virulence of the strain and the host's immune response.
Clinical Manifestations of S. Aureus Skin Infections
The clinical presentation of S. aureus infections varies considerably, depending on several factors, including the virulence of the strain, the site of infection, and the host's immune status. Common manifestations include:
Impetigo: A Superficial Infection
Impetigo is a highly contagious superficial skin infection, commonly affecting children. It is characterized by the formation of honey-colored crusts on the skin, primarily affecting the face and extremities. This infection primarily involves the epidermis.
Folliculitis: Infection of the Hair Follicles
Folliculitis involves the infection of hair follicles, leading to small, pus-filled bumps. This infection can be localized or widespread, and the severity can range from mild to severe. The deeper involvement of the hair follicle places this infection at the interface between the epidermis and dermis.
Cellulitis: A Deeper Dermal Infection
Cellulitis is a spreading infection affecting the dermis and subcutaneous tissue. It's characterized by redness, swelling, pain, and warmth at the site of infection. Cellulitis can progress rapidly and potentially lead to serious complications if left untreated. The deeper involvement of the dermis highlights the significant impact of S. aureus on this skin layer.
Abscesses: Localized Collections of Pus
Abscesses are localized collections of pus, typically resulting from a deeper infection. These are characterized by localized swelling, pain, and tenderness. Abscesses can form in various locations, including the skin, subcutaneous tissue, and deeper structures. Their formation often involves the dermis and subcutaneous tissue.
Necrotizing Fasciitis: A Life-Threatening Infection
Necrotizing fasciitis is a severe, life-threatening infection characterized by rapid destruction of the soft tissues, including the fascia, subcutaneous tissue, and muscles. This condition is often polymicrobial, but S. aureus is frequently involved. Necrotizing fasciitis showcases the extreme destructive potential of S. aureus at the dermal and deeper tissue layers.
Diagnosis and Treatment of S. Aureus Skin Infections
Accurate diagnosis of S. aureus skin infections typically involves clinical examination, coupled with microbiological testing. Swabs from the infected area are cultured to isolate and identify the causative organism. Gram staining can provide rapid preliminary identification. Further tests may be employed to determine the susceptibility of the isolate to various antibiotics.
Treatment options depend on the severity and location of the infection. Mild infections, such as impetigo, may respond to topical antibiotics. More severe infections, like cellulitis or abscesses, often require systemic antibiotic therapy. Abscesses may require incision and drainage to remove the pus. In cases of necrotizing fasciitis, immediate surgical debridement and broad-spectrum antibiotic therapy are crucial to save the patient's life.
Prevention of S. Aureus Skin Infections
Preventing S. aureus skin infections involves several strategies:
-
Good hygiene: Regular handwashing, particularly after contact with potentially contaminated surfaces, is essential in preventing the spread of S. aureus.
-
Wound care: Proper wound care, including cleaning and covering wounds, is crucial in preventing infection.
-
Avoidance of sharing personal items: Sharing towels, razors, and other personal items can facilitate the spread of S. aureus.
-
Treatment of colonized individuals: Individuals carrying S. aureus in their nasal passages or on their skin can be treated with topical or systemic antibiotics to reduce colonization and prevent infection.
Conclusion
Staphylococcus aureus remains a significant cause of skin and soft tissue infections, impacting both the epidermis and dermis. Its ability to adhere, invade, and evade the host's immune system, coupled with its production of a diverse array of virulence factors, contribute to its pathogenic potential. A thorough understanding of S. aureus's mechanisms of pathogenesis, coupled with effective diagnostic tools and treatment strategies, is critical in managing the burden of these infections and minimizing their impact on public health. Further research is ongoing to understand the intricacies of the host-pathogen interaction and to develop novel therapeutic strategies to combat this persistent pathogen. Continued emphasis on preventative measures, such as good hygiene practices and proper wound care, remains vital in reducing the incidence of S. aureus skin infections. The fight against this resilient bacterium requires a multifaceted approach, combining advanced research with practical public health initiatives.
Latest Posts
Latest Posts
-
Indicate The Three Items That Describe Glycogen
Mar 17, 2025
-
Cyclic Amp Phosphodiesterase Is An Enzyme That Catalyzes The Conversion
Mar 17, 2025
-
The Usual Starting Point For A Master Budget Is
Mar 17, 2025
-
When Preparing To Begin A Speech Positive Nervousness Refers To
Mar 17, 2025
-
An Increase In Income Will Blank
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about Staphylococcus Aureus Produces A Of The Epidermis And Dermis. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
