Radiolucent Lesion Apical To Tooth 30
Holbox
Mar 18, 2025 · 6 min read
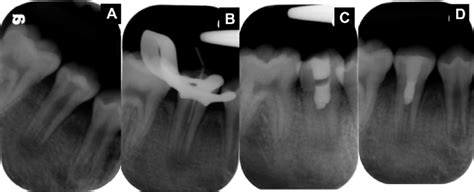
Table of Contents
Radiolucent Lesion Apical to Tooth #30: A Comprehensive Overview
A radiolucent lesion apical to tooth #30, meaning a dark area on a dental X-ray located at the root tip of the lower right first molar, presents a significant diagnostic challenge for dentists. This article delves into the various potential causes of such a lesion, emphasizing the importance of a thorough clinical examination, radiographic analysis, and potentially further investigations to arrive at an accurate diagnosis and appropriate treatment plan.
Understanding the Basics
Before exploring specific pathologies, let's establish a fundamental understanding. A radiolucent lesion appears dark on a dental radiograph because it is less dense than the surrounding tooth structure and bone. The location, "apical to tooth #30," indicates its proximity to the root apex, the tip of the tooth root. This anatomical position strongly suggests a relationship to the tooth itself, though not exclusively. The size and shape of the lesion are crucial diagnostic factors.
Key Diagnostic Steps
Diagnosing the cause of a radiolucent lesion apical to tooth #30 requires a systematic approach:
-
Detailed Medical and Dental History: This includes inquiries about pain, swelling, history of trauma, previous dental procedures on tooth #30 or adjacent teeth, systemic illnesses, and family history of dental anomalies.
-
Thorough Clinical Examination: This encompasses a visual inspection of the soft tissues (checking for swelling, fistula, or discoloration), palpation (assessing for tenderness or fluctuance), and periodontal probing (measuring pocket depths around tooth #30). The dentist will carefully examine tooth #30 for caries, fractures, mobility, and periapical inflammation.
-
Radiographic Analysis: Periapical radiographs provide the primary imaging modality for evaluating this type of lesion. Ideally, multiple radiographs from different angles (e.g., bitewing and panoramic) might be necessary to accurately assess the lesion's size, shape, borders, and relationship to surrounding structures. Additional imaging techniques, such as cone-beam computed tomography (CBCT), may be employed for complex cases requiring a three-dimensional assessment.
Differential Diagnosis: Potential Causes
The differential diagnosis of a radiolucent lesion apical to tooth #30 encompasses a range of possibilities, each with its unique characteristics and treatment implications:
1. Periapical Cyst (Radicular Cyst)
This is often the most common cause of a radiolucent lesion at the root apex. It develops as a result of pulpal necrosis and subsequent inflammation. The cyst is a fluid-filled sac lined by epithelium, and its size can vary considerably.
-
Radiographic Appearance: Well-defined, round-to-oval radiolucency associated with the root apex of a non-vital tooth. The lesion may appear unilocular (single chamber) or multilocular (multiple chambers).
-
Clinical Presentation: Often asymptomatic in early stages. Larger cysts may cause swelling, pain, or expansion of the alveolar bone.
-
Treatment: Surgical removal (apicoectomy) or endodontic treatment (root canal therapy) followed by observation.
2. Periapical Granuloma
A periapical granuloma is an inflammatory lesion formed in response to pulpal necrosis. Unlike a cyst, it lacks an epithelial lining.
-
Radiographic Appearance: Irregular, ill-defined radiolucency associated with the apex of a non-vital tooth. It's usually smaller than a periapical cyst.
-
Clinical Presentation: Frequently asymptomatic. Pain or swelling may occur if the granuloma becomes infected.
-
Treatment: Root canal therapy is usually sufficient. Surgical intervention might be necessary for persistent or large granulomas.
3. Abscess
An abscess is a localized collection of pus caused by bacterial infection. Periapical abscesses can arise from untreated or inadequately treated caries, periodontal disease, or trauma.
-
Radiographic Appearance: May or may not show a distinct radiolucency in early stages. As the abscess develops, it can cause bone resorption, creating a radiolucent area.
-
Clinical Presentation: Characterized by severe, throbbing pain, swelling, tenderness to palpation, and sometimes a draining fistula (a small opening through the gingiva).
-
Treatment: Requires prompt drainage of the pus and often involves endodontic therapy or extraction. Antibiotics may be necessary to control the infection.
4. Residual Cyst
This occurs after extraction of a tooth, when the periapical cyst is not completely removed during the extraction process.
-
Radiographic Appearance: Radiolucency in the area where the tooth was previously located. Resembles a periapical cyst.
-
Clinical Presentation: Usually asymptomatic but can occasionally cause swelling or pain.
-
Treatment: Surgical excision.
5. Lateral Periodontal Cyst
This rare cyst develops in the lateral periodontal tissues, between the root and the alveolar bone. Unlike periapical cysts, it is not directly related to the tooth's pulp.
-
Radiographic Appearance: Well-defined, ovoid radiolucency typically located along the lateral root surface.
-
Clinical Presentation: Usually asymptomatic and discovered incidentally on routine radiographic examination.
-
Treatment: Surgical enucleation (removal).
6. Traumatic Bone Cyst (Simple Bone Cyst)
This pseudocyst (not a true cyst) is thought to be a result of trauma or bone healing disturbances.
-
Radiographic Appearance: Well-defined, round or oval radiolucency with a sclerotic border (a dense, white line).
-
Clinical Presentation: Generally asymptomatic; often discovered incidentally.
-
Treatment: Curettage (scraping) of the cyst cavity is usually sufficient.
7. Odontogenic Keratocyst
This is a more aggressive cyst of odontogenic origin, meaning it originates from the tissues that form teeth.
-
Radiographic Appearance: Well-defined, unilocular or multilocular radiolucency. Can be quite large.
-
Clinical Presentation: May be asymptomatic or cause expansion of the bone. Has a high recurrence rate.
-
Treatment: Surgical enucleation with careful removal of the cyst lining to prevent recurrence.
8. Ameloblastoma
This is a benign but locally aggressive tumor of odontogenic origin.
-
Radiographic Appearance: Multilocular radiolucency with a soap-bubble appearance.
-
Clinical Presentation: Slow-growing, can cause expansion and displacement of teeth.
-
Treatment: Surgical resection, often requiring significant bone removal.
9. Other Possibilities
Less common causes include: adenomatoid odontogenic tumor, calcifying epithelial odontogenic tumor, and central giant cell granuloma. These require specialized diagnostic procedures and treatment plans.
Importance of Accurate Diagnosis and Treatment
The accurate diagnosis of a radiolucent lesion apical to tooth #30 is crucial for determining the appropriate treatment. Failing to diagnose and treat a serious condition, such as an aggressive tumor or recurrent cyst, can lead to significant complications, including facial deformity, infection spread, and potential impairment of adjacent structures.
Role of the Interdisciplinary Approach
Complex cases may require an interdisciplinary approach, involving specialists such as oral and maxillofacial surgeons, endodontists, and pathologists. This collaborative approach ensures optimal management of the case, maximizing the chances of successful treatment and minimizing the risk of complications.
The Role of Biopsy and Histopathology
In many cases, a definitive diagnosis can only be reached through a biopsy—a small tissue sample taken from the lesion and examined under a microscope by a pathologist. This is particularly important if the radiographic and clinical findings are inconclusive or suggestive of a more serious pathology.
Monitoring and Follow-up Care
After treatment, regular follow-up appointments are necessary to monitor the healing process and detect any potential recurrence or complications. Radiographic examinations are often conducted at scheduled intervals to assess the changes in the lesion's size and appearance.
Conclusion: A Multifaceted Diagnostic Challenge
A radiolucent lesion apical to tooth #30 is a common finding in dental practice, but it is also a diagnostic challenge due to the wide range of potential underlying causes. A careful consideration of the patient's history, a thorough clinical examination, detailed radiographic analysis, and—when necessary—biopsy and histopathology are all crucial steps in establishing an accurate diagnosis and creating a personalized treatment plan that ensures the best possible outcomes for the patient. Remember, early detection and prompt treatment are essential for preventing complications and preserving oral health. This comprehensive overview provides a broad understanding, but always consult with a qualified dental professional for any concerns or issues related to your oral health.
Latest Posts
Latest Posts
-
A Clarinetist Setting Out For A Performance
Mar 18, 2025
-
645 Is The Same As What Percent
Mar 18, 2025
-
How To Cite Survey In Mla
Mar 18, 2025
-
Specific Performance Is A Remedy Which Is Always Available In
Mar 18, 2025
-
How Does Deflation Impact The Burden Of Debt For Borrowers
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Radiolucent Lesion Apical To Tooth 30 . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
