Main Bacteria Killer During Acute Infections
Holbox
Mar 19, 2025 · 6 min read
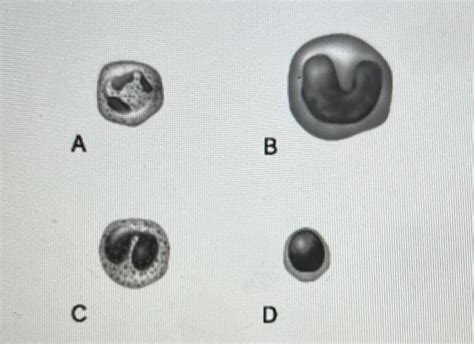
Table of Contents
Main Bacteria Killers During Acute Infections: A Deep Dive into the Body's Defenses and Medical Interventions
Acute infections, characterized by their rapid onset and relatively short duration, pose a significant threat to human health. Understanding the body's natural defenses and the medical interventions used to combat these infections is crucial for effective treatment and prevention. This article will delve into the key players in eliminating bacteria during acute infections, exploring both the innate and adaptive immune systems, as well as the role of antibiotics and other therapeutic strategies.
The Body's First Line of Defense: Innate Immunity
The innate immune system is our body's immediate, non-specific response to invading pathogens, including bacteria. This rapid-response system acts as the first line of defense, preventing the establishment of infection and limiting its spread. Key components of the innate immune response against bacteria during acute infections include:
1. Physical Barriers: The Body's Walls
The skin and mucous membranes form a formidable physical barrier, preventing bacterial entry. The skin's acidity and the constant shedding of skin cells inhibit bacterial colonization. Mucous membranes, lining the respiratory, gastrointestinal, and genitourinary tracts, trap and remove bacteria through the action of cilia and mucus flow. Damage to these barriers, such as through wounds or burns, significantly increases the risk of infection.
2. Chemical Barriers: A Toxic Cocktail
Chemical defenses contribute significantly to innate immunity. The acidic environment of the stomach destroys many ingested bacteria. Lysozyme, an enzyme found in tears, saliva, and mucus, breaks down bacterial cell walls. Defensins, antimicrobial peptides, directly kill bacteria by disrupting their cell membranes. These chemical barriers are constantly active, providing continuous protection against bacterial invasion.
3. Cellular Defenses: The Cellular Army
If bacteria breach the physical and chemical barriers, the cellular components of the innate immune system spring into action. These include:
-
Phagocytes: These cells, including neutrophils, macrophages, and dendritic cells, engulf and destroy bacteria through phagocytosis. Neutrophils are the first responders, arriving at the infection site within minutes. Macrophages reside in tissues and are long-lived phagocytes that also play a crucial role in antigen presentation to the adaptive immune system. Dendritic cells capture and present antigens to initiate the adaptive immune response.
-
Natural Killer (NK) Cells: These lymphocytes identify and kill infected or cancerous cells, preventing the spread of infection. They achieve this through the release of cytotoxic granules that induce apoptosis (programmed cell death) in target cells.
-
Complement System: This complex system of proteins enhances the ability of antibodies and phagocytes to clear pathogens. Complement proteins can directly kill bacteria through membrane attack complexes (MACs), which create pores in bacterial cell membranes, leading to cell lysis. They also promote inflammation and enhance phagocytosis through opsonization (coating bacteria to make them more easily recognized by phagocytes).
-
Inflammation: Inflammation is a crucial part of the innate immune response. It's characterized by redness, swelling, heat, and pain. Inflammation recruits immune cells to the infection site, isolates the pathogen, and promotes tissue repair. While uncomfortable, inflammation is a vital process in clearing infection.
The Adaptive Immune System: A Targeted Response
While the innate immune system provides immediate protection, the adaptive immune system mounts a more specific and long-lasting response. This system learns to recognize and eliminate specific pathogens, providing immunological memory for future encounters. Key players in the adaptive immune response against bacterial infections include:
1. B Lymphocytes (B Cells): Antibody Production
B cells produce antibodies, specialized proteins that bind to specific bacterial antigens (surface molecules). This binding neutralizes the bacteria, preventing them from infecting cells, and marks them for destruction by phagocytes or the complement system. B cells differentiate into plasma cells, which produce large quantities of antibodies, and memory B cells, which provide long-term immunity.
2. T Lymphocytes (T Cells): Cellular Warfare
T cells play a crucial role in eliminating infected cells and coordinating the immune response. Several types of T cells are involved:
-
Helper T cells (Th cells): These cells orchestrate the immune response by releasing cytokines, signaling molecules that activate other immune cells, such as B cells and macrophages. Different subsets of Th cells (Th1, Th2, Th17) play specific roles in different types of infections.
-
Cytotoxic T cells (Tc cells): These cells recognize and kill infected cells by releasing cytotoxic granules containing perforin and granzymes, inducing apoptosis. They are particularly important in eliminating bacteria that have invaded host cells.
-
Regulatory T cells (Treg cells): These cells help to suppress the immune response and prevent excessive inflammation, maintaining immune homeostasis. They prevent autoimmunity and limit collateral damage to host tissues.
Medical Interventions: Antibiotics and Beyond
When the body's immune system is overwhelmed, or the infection is particularly severe, medical intervention is often necessary. Antibiotics are the cornerstone of bacterial infection treatment, but other therapeutic strategies play a critical role:
1. Antibiotics: The Bacterial Killers
Antibiotics are drugs that kill or inhibit the growth of bacteria. They work by targeting various bacterial structures and processes, such as cell wall synthesis, protein synthesis, DNA replication, and folic acid metabolism. Different classes of antibiotics have different mechanisms of action and target different types of bacteria. The choice of antibiotic depends on the type of bacteria causing the infection, its susceptibility to different antibiotics, and the patient's overall health.
Important Note: The overuse and misuse of antibiotics have led to the rise of antibiotic-resistant bacteria, a major public health concern. It's crucial to use antibiotics judiciously, only when necessary and as prescribed by a healthcare professional.
2. Other Therapeutic Strategies
Beyond antibiotics, several other therapeutic strategies are used to combat acute bacterial infections:
-
Antiviral medications: In cases where viral co-infections complicate bacterial infections, antiviral drugs may be necessary.
-
Immunomodulators: These drugs modify the immune response, either boosting it or suppressing it, depending on the specific needs of the patient. For instance, immunoglobulins can provide passive immunity to individuals with weakened immune systems.
-
Supportive Care: Supportive care focuses on maintaining the patient's overall health and well-being during the infection. This includes managing symptoms, such as fever and pain, providing adequate hydration and nutrition, and monitoring vital signs. In severe cases, hospitalization may be required to provide intensive supportive care.
-
Surgical Debridement: In cases of severe localized infections, surgical removal of infected tissue may be necessary to prevent the spread of infection and promote healing.
-
Drainage of Abscesses: Abscesses, localized collections of pus, need to be drained to allow for effective treatment of the infection. This can be achieved through surgical incision or needle aspiration.
Conclusion: A Complex Battle for Health
The fight against acute bacterial infections is a complex interplay between the body's innate and adaptive immune systems and medical interventions. Understanding the mechanisms of bacterial pathogenesis and the body's defenses is crucial for developing effective treatments and prevention strategies. The responsible use of antibiotics, coupled with supportive care and other therapeutic approaches, remains essential for combating these infections and safeguarding public health. Further research into novel antibiotics, immunotherapies, and vaccines is vital to address the growing challenge of antibiotic resistance and improve patient outcomes. The battle against bacteria is an ongoing one, requiring continuous vigilance and innovation.
Latest Posts
Latest Posts
-
What Is The Difference Between Tough And Tuff
Mar 19, 2025
-
Locking Out Tagging Out Refers To The Practice Of
Mar 19, 2025
-
John Is Rollerblading Down A Long
Mar 19, 2025
-
Hydrolysis Of Sucrose A Disaccharide Results In
Mar 19, 2025
-
What Is The Difference Between Mutualism And Synergism
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about Main Bacteria Killer During Acute Infections . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
