Informed Consent Means Clearly Explaining All Of The Following Except
Holbox
Mar 14, 2025 · 5 min read
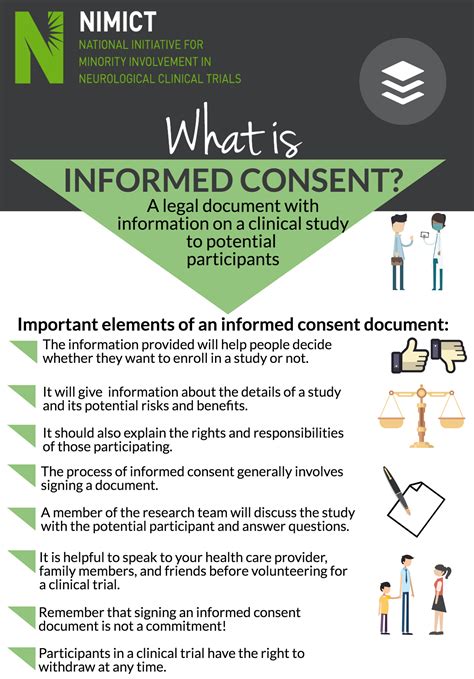
Table of Contents
Informed Consent: Clearly Explaining Everything Except…
Informed consent is a cornerstone of ethical medical practice and research. It’s a process, not just a signature on a form, that ensures individuals understand the implications of medical procedures or research participation before agreeing to them. But what exactly isn't included in this crucial process? Let's delve into the specifics of informed consent and pinpoint the exclusion.
The Pillars of Informed Consent
Before we address the exception, let's solidify our understanding of what informed consent does encompass. It's built upon several key pillars:
1. Disclosure: This is the most fundamental aspect. Healthcare providers or researchers have a responsibility to clearly and comprehensively explain all relevant information to the potential participant. This includes:
- The nature of the procedure or research: What will be done? What are the steps involved? What are the expected outcomes?
- The risks and benefits: Both the potential positive and negative consequences must be disclosed, including the probability of each occurring. This should be presented in a way that is easily understood, avoiding overly technical jargon.
- Alternatives: Are there other options available? What are the risks and benefits of those alternatives? This allows the individual to make an informed comparison.
- The right to refuse or withdraw: Participants must understand that they have the absolute right to decline participation at any point, even after they've initially agreed, without facing any negative consequences. This also applies to the right to withdraw from research at any stage.
- Confidentiality: How will the participant's privacy be protected? Will their personal information be kept confidential? What are the limitations of confidentiality (e.g., mandatory reporting of certain conditions)?
2. Comprehension: The information disclosed must be easily understandable. The complexity of medical information can be daunting for many individuals. Therefore, providers must ensure the language used is clear, concise, and free from technical jargon. Visual aids, simplified explanations, and the use of plain language are crucial for effective comprehension. The provider should assess the individual's understanding through open-ended questions and ensure they are comfortable with the information.
3. Voluntariness: The decision to participate or not must be entirely free from coercion, pressure, or manipulation. Individuals must feel empowered to make their own choices without feeling obligated or influenced by others. This is particularly important in vulnerable populations, where coercion may be more likely.
4. Competence: The individual must possess the capacity to understand the information presented and make a reasoned decision. This involves considering factors such as age, mental capacity, and cognitive abilities. If an individual lacks competence, informed consent must be obtained from a legally authorized representative.
The Exception: Guaranteeing Specific Outcomes
Now, let's address the crucial exclusion: Informed consent does not guarantee a specific outcome.
This is a vital distinction. While informed consent mandates a thorough explanation of potential risks and benefits, it cannot promise a particular result. Medical procedures and research participation are inherently uncertain. Even with the best care and the most promising research, there is always a possibility of unforeseen complications or negative outcomes.
Why is this important?
Overpromising or creating unrealistic expectations during the informed consent process can lead to several serious ethical and legal issues:
- Breach of trust: If a healthcare provider or researcher makes promises they cannot keep, it erodes the patient's or participant's trust. This can have devastating consequences on the doctor-patient relationship.
- Legal liability: Guaranteeing a specific outcome can create grounds for malpractice lawsuits if the anticipated results are not achieved.
- Exploitation of vulnerability: Patients or research participants who are particularly vulnerable may be more susceptible to believing unrealistic promises. This can be especially harmful.
- Compromised autonomy: If individuals are led to believe a procedure guarantees a certain outcome, their autonomy – their ability to make informed decisions – is compromised.
Examples of unrealistic guarantees:
- "This surgery will completely cure your cancer."
- "This medication will eliminate all of your symptoms."
- "This research study guarantees you will experience significant improvements."
Instead of guarantees, providers should focus on providing realistic expectations and probabilities. They should emphasize that outcomes are variable and may not always meet the hoped-for results.
Strengthening the Informed Consent Process
Several strategies can enhance the effectiveness of the informed consent process and ensure individuals understand the uncertainties involved:
- Use plain language: Avoid medical jargon and technical terms. Employ simple, clear language that everyone can understand.
- Provide visual aids: Charts, diagrams, and infographics can help clarify complex information.
- Use a multi-modal approach: Combine verbal explanations with written materials and visual aids.
- Allow ample time for questions: Encourage participants to ask questions and ensure they have a thorough understanding before proceeding.
- Document the process meticulously: Maintain comprehensive records of the informed consent discussions, including any questions asked and answers provided.
- Offer interpreter services if needed: Ensure language barriers don't impede understanding.
- Utilize shared decision-making models: Engage patients actively in the decision-making process, promoting collaborative care.
- Regularly review and update consent forms: Ensure the forms are current, reflect the latest research, and are easy to understand.
- Provide ongoing support and communication: Maintain open communication throughout the process, addressing any concerns or questions.
Conclusion: Transparency and Realistic Expectations
Informed consent is a crucial ethical and legal requirement in healthcare and research. It emphasizes transparency, empowering individuals to make informed decisions about their health and participation in research. However, it's crucial to remember that informed consent does not, and cannot, guarantee a specific outcome. By focusing on clear communication, realistic expectations, and a patient-centered approach, we can strengthen the informed consent process, fostering trust and promoting ethical practices. Understanding this key exception – the inability to guarantee specific outcomes – is vital for maintaining the integrity of informed consent and ensuring individuals make truly autonomous decisions. The emphasis should be on a shared understanding of the process, risks, benefits, and the inherent uncertainties involved, allowing for true self-determination in healthcare choices.
Latest Posts
Latest Posts
-
On December 31 2021 Coolwear Inc
Mar 15, 2025
-
Did Not Load Results Should Be Rated Fails To Meet
Mar 15, 2025
-
Which Tools Would You Use To Make Header
Mar 15, 2025
-
A Solid Cylindrical Conducting Shell Of Inner Radius
Mar 15, 2025
-
A High End Auto Dealer Wants To Identify Qualified Buyers
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about Informed Consent Means Clearly Explaining All Of The Following Except . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
