Bradycardia Is Most Commonly Seen With Which Intrapartum Complications
Holbox
Mar 25, 2025 · 7 min read
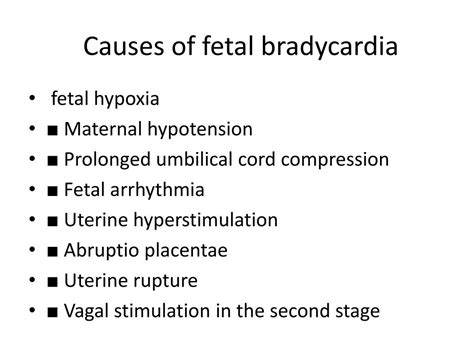
Table of Contents
- Bradycardia Is Most Commonly Seen With Which Intrapartum Complications
- Table of Contents
- Bradycardia: A Deep Dive into Intrapartum Complications and Fetal Heart Rate Monitoring
- Intrapartum Complications Frequently Associated with Fetal Bradycardia
- 1. Uterine Factors:
- 2. Umbilical Cord Complications:
- 3. Placental Abnormalities:
- 4. Maternal Factors:
- 5. Fetal Factors:
- The Role of Electronic Fetal Monitoring (EFM)
- Clinical Management of Fetal Bradycardia
- Conclusion
- Latest Posts
- Latest Posts
- Related Post
Bradycardia: A Deep Dive into Intrapartum Complications and Fetal Heart Rate Monitoring
Bradycardia, characterized by a fetal heart rate (FHR) below 110 beats per minute (bpm) for at least 10 minutes, is a significant indicator of potential intrapartum complications. Its presence necessitates immediate attention and intervention from healthcare professionals to ensure the well-being of both the mother and the fetus. Understanding the specific intrapartum complications most commonly associated with bradycardia is crucial for effective management and improved perinatal outcomes. This article explores the intricate relationship between bradycardia and various intrapartum events, providing a comprehensive overview of the underlying mechanisms and clinical implications.
Intrapartum Complications Frequently Associated with Fetal Bradycardia
Several intrapartum complications are strongly linked with the onset of fetal bradycardia. These complications can be broadly classified into categories based on their underlying pathophysiological mechanisms, allowing for a more systematic understanding of this critical fetal condition.
1. Uterine Factors:
Uterine Hyperstimulation/Tachysystole: This condition, characterized by excessively frequent and strong uterine contractions, is a significant cause of fetal bradycardia. The intense contractions can compromise uteroplacental blood flow, leading to fetal hypoxia and subsequent bradycardia. The reduced blood flow deprives the fetus of essential oxygen and nutrients, causing a decrease in the heart rate.
-
Mechanism: Sustained uterine contractions restrict blood flow through the intervillous spaces of the placenta, reducing oxygen and nutrient delivery to the fetus. This hypoxia triggers the fetal baroreceptor reflex, leading to bradycardia as the body attempts to conserve oxygen.
-
Clinical Significance: Continuous electronic fetal monitoring (EFM) is crucial for detecting tachysystole and associated bradycardia. Management usually involves reducing uterine activity through interventions such as administering tocolytic medications (e.g., terbutaline, magnesium sulfate) or altering the maternal position.
Uterine Rupture: A complete or partial rupture of the uterus is a life-threatening complication that frequently presents with severe fetal bradycardia. The rupture disrupts blood flow to the fetus, causing acute hypoxia and potentially leading to fetal distress or death.
-
Mechanism: Uterine rupture interrupts the placental circulation, leading to immediate and profound fetal hypoxia. The resulting bradycardia is often profound and persistent.
-
Clinical Significance: Uterine rupture is a surgical emergency requiring immediate intervention. Clinical presentation often includes severe abdominal pain, maternal hypotension, and signs of hypovolemic shock. Fetal bradycardia is a critical warning sign.
2. Umbilical Cord Complications:
Umbilical Cord Compression: Compression of the umbilical cord, either by the presenting part or by a nuchal cord (cord around the neck), significantly reduces blood flow to the fetus. This results in hypoxia and subsequent bradycardia. Prolonged or severe compression can lead to severe fetal acidosis and irreversible damage.
-
Mechanism: Compression of the umbilical cord restricts the flow of oxygenated blood to the fetus and impedes the return of deoxygenated blood. This reduction in blood flow triggers the fetal baroreceptor reflex, leading to a decrease in the FHR.
-
Clinical Significance: Identifying and relieving cord compression is critical. Changes in maternal position, amnioinfusion (infusion of fluid into the amniotic cavity to relieve compression), or immediate cesarean section may be required.
Umbilical Cord Prolapse: This occurs when the umbilical cord descends into the vagina or cervix before the presenting part of the fetus. The cord can become compressed between the presenting part and the maternal pelvis, leading to severe and potentially fatal fetal bradycardia.
-
Mechanism: The cord becomes severely compressed, resulting in acute and profound hypoxia. The resulting bradycardia is often dramatic and requires immediate intervention.
-
Clinical Significance: Umbilical cord prolapse is a medical emergency requiring immediate intervention, typically an urgent cesarean delivery to prevent fetal asphyxia.
3. Placental Abnormalities:
Placental Abruption: This involves premature separation of the placenta from the uterine wall, disrupting blood flow to the fetus. Placental abruption is a serious complication that can cause severe fetal bradycardia, fetal distress, and maternal hemorrhage.
-
Mechanism: The detachment of the placenta disrupts the exchange of oxygen and nutrients between the mother and the fetus, leading to acute hypoxia and subsequent bradycardia.
-
Clinical Significance: Management depends on the severity of the abruption and the fetal condition. Close monitoring of maternal vital signs and fetal heart rate, along with blood replacement and potential emergency cesarean section are crucial.
Placenta Previa: In placenta previa, the placenta implants over or near the cervix, obstructing the fetal passage. While not directly causing bradycardia, bleeding associated with placenta previa can lead to hypovolemia and maternal hypotension, potentially causing fetal hypoxia and secondary bradycardia.
-
Mechanism: Bleeding associated with placenta previa can lead to maternal hypovolemia and hypotension, reducing uterine blood flow and causing fetal hypoxia, consequently triggering bradycardia.
-
Clinical Significance: Careful monitoring for bleeding is paramount. Management often involves close monitoring, blood transfusions if necessary, and potentially cesarean delivery.
4. Maternal Factors:
Maternal Hypotension: A significant drop in maternal blood pressure can compromise uteroplacental perfusion, leading to fetal hypoxia and bradycardia. Hypotension can occur due to various factors such as hemorrhage, epidural anesthesia, or severe dehydration.
-
Mechanism: Reduced maternal blood pressure limits blood flow to the uterus, decreasing oxygen and nutrient delivery to the fetus, leading to hypoxia and bradycardia.
-
Clinical Significance: Treating maternal hypotension is crucial. Interventions include fluid resuscitation, repositioning the mother, and managing the underlying cause of the hypotension.
5. Fetal Factors:
Fetal Heart Block: This condition, characterized by a slowed conduction of electrical impulses within the fetal heart, can cause prolonged fetal bradycardia. Fetal heart block can be congenital or acquired.
-
Mechanism: Impaired conduction of electrical impulses through the fetal heart leads to a reduction in the heart rate.
-
Clinical Significance: Management depends on the severity of the heart block and the fetal condition. Close monitoring and potential interventions to support the fetal circulation may be necessary.
Fetal Infections (e.g., Chorioamnionitis): Infection within the amniotic cavity can cause fetal tachycardia or bradycardia, depending on the severity and progression of the infection. Severe infections can lead to fetal hypoxia and bradycardia.
-
Mechanism: Infection can lead to inflammation and compromise of placental function, resulting in fetal hypoxia and bradycardia.
-
Clinical Significance: Treatment focuses on addressing the underlying infection with antibiotics. Close monitoring of the fetal heart rate and maternal condition is crucial.
Fetal Acidosis: Increased levels of acidity in the fetal blood can affect fetal heart function, leading to bradycardia. Fetal acidosis is often associated with hypoxia.
-
Mechanism: Acidosis alters the electrochemical gradients within the fetal heart, affecting the ability of the heart to conduct electrical impulses effectively and leading to bradycardia.
-
Clinical Significance: Treatment focuses on addressing the underlying cause of the acidosis, such as hypoxia or infection.
The Role of Electronic Fetal Monitoring (EFM)
Electronic fetal monitoring (EFM) plays a pivotal role in detecting and managing fetal bradycardia. Continuous monitoring allows for the early identification of changes in the fetal heart rate, facilitating timely interventions to mitigate potential adverse outcomes. EFM enables healthcare professionals to identify patterns and trends in the FHR, providing valuable information about the fetal condition and the presence of potential complications. The interpretation of EFM tracings requires considerable expertise and experience, emphasizing the importance of ongoing education and training for healthcare providers.
Clinical Management of Fetal Bradycardia
The management of fetal bradycardia depends on several factors, including the severity, duration, and underlying cause of the bradycardia. Immediate interventions may be necessary to ensure the safety of both the mother and the fetus. These interventions may include:
- Change in maternal position: Changing the mother's position can sometimes relieve umbilical cord compression.
- Administration of oxygen: Providing supplemental oxygen to the mother can improve uteroplacental blood flow.
- Fluid bolus: Administering intravenous fluids to the mother can help improve maternal blood volume and blood pressure.
- Tocolysis: Medications such as terbutaline or magnesium sulfate can be used to reduce uterine contractions.
- Amnioinfusion: Infusion of fluid into the amniotic cavity can help alleviate umbilical cord compression.
- Cesarean section: Emergency cesarean delivery may be necessary in cases of severe or prolonged bradycardia, particularly when associated with conditions such as umbilical cord prolapse or uterine rupture.
Conclusion
Fetal bradycardia during labor is a serious event requiring prompt assessment and management. Its association with various intrapartum complications underscores the importance of continuous fetal monitoring and a multidisciplinary approach to care. Understanding the underlying mechanisms and potential causes of fetal bradycardia is essential for healthcare providers to effectively manage this critical condition and improve perinatal outcomes. The timely identification and appropriate management of the underlying causes are crucial in minimizing the risks to both mother and baby. Continued research and advancements in technology will further enhance our understanding and ability to manage this challenging aspect of obstetrical care.
Latest Posts
Latest Posts
-
Campaigning Its A Process Answer Key
Mar 26, 2025
-
Rn Pharmacology Online Practice 2023 B
Mar 26, 2025
-
A Sales Rep Is Displaying His Companys Newest Smartwatches
Mar 26, 2025
-
Consider The Following Scenarios Which Behaviors Must Be Reported
Mar 26, 2025
-
Which Of The Following Is Correct
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Bradycardia Is Most Commonly Seen With Which Intrapartum Complications . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
