Activation Of Sympathetic Nerves That Innervate Lung Tissue Results In
Holbox
Mar 30, 2025 · 6 min read
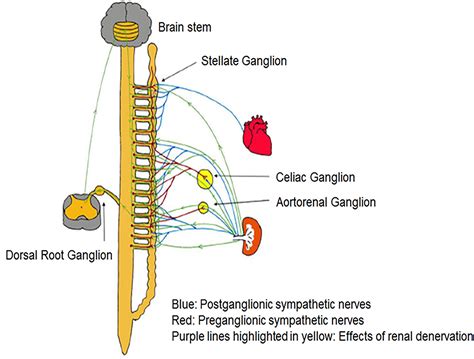
Table of Contents
- Activation Of Sympathetic Nerves That Innervate Lung Tissue Results In
- Table of Contents
- Activation of Sympathetic Nerves that Innervate Lung Tissue Results In: A Deep Dive into Bronchodilation and Beyond
- The Sympathetic Nervous System and Lung Innervation
- Neurotransmitters and Receptors: The Key Players
- Bronchodilation: The Primary Effect of Sympathetic Activation
- Clinical Significance of Bronchodilation
- Beyond Bronchodilation: Other Effects of Sympathetic Activation in the Lungs
- Modulation of Airway Secretion
- Pulmonary Vascular Tone
- Influence on Lung Immune Cells
- Interactions with Other Systems
- Clinical Implications and Future Directions
- Conclusion
- Latest Posts
- Latest Posts
- Related Post
Activation of Sympathetic Nerves that Innervate Lung Tissue Results In: A Deep Dive into Bronchodilation and Beyond
The intricate network of nerves within the lungs plays a crucial role in regulating respiratory function. Among these, the sympathetic nervous system, a key component of the autonomic nervous system, exerts significant influence on various aspects of lung physiology. Activation of sympathetic nerves that innervate lung tissue primarily results in bronchodilation, but its effects extend far beyond this singular function, impacting airway secretion, vascular tone, and even immune responses within the pulmonary system. This article will delve into the complex mechanisms and consequences of sympathetic activation in the lungs, exploring its physiological impact and clinical implications.
The Sympathetic Nervous System and Lung Innervation
The sympathetic nervous system, often associated with the "fight-or-flight" response, uses norepinephrine (noradrenaline) as its primary neurotransmitter. Sympathetic fibers reach the lungs via the pulmonary plexus, a network of nerve fibers that runs alongside the pulmonary arteries and bronchi. These fibers don't directly innervate all lung cells; instead, they primarily target smooth muscle cells in the airways and blood vessels, as well as some secretory cells and immune cells within the lung parenchyma.
Neurotransmitters and Receptors: The Key Players
The effects of sympathetic activation are mediated by the interaction of norepinephrine with adrenergic receptors located on target cells. In the lungs, the primary receptors involved are β2-adrenergic receptors. These receptors are predominantly found on airway smooth muscle cells. Stimulation of β2-adrenergic receptors by norepinephrine leads to a cascade of intracellular events, ultimately resulting in relaxation of the airway smooth muscle and bronchodilation.
While β2-adrenergic receptors are the predominant players in mediating bronchodilation, other adrenergic receptors, such as α1-adrenergic receptors (found on some airway smooth muscle and blood vessels), and β1-adrenergic receptors (primarily found on cardiac tissue but with some presence in pulmonary vasculature) also play roles, although their contributions to the overall effects of sympathetic activation are less prominent in broncho-pulmonary physiology.
Bronchodilation: The Primary Effect of Sympathetic Activation
The most well-established effect of sympathetic nerve activation in the lungs is bronchodilation, the widening of the airways. This occurs due to the relaxation of the smooth muscle surrounding the bronchi and bronchioles. This relaxation is triggered by the binding of norepinephrine to β2-adrenergic receptors. The subsequent intracellular signaling pathway involves the activation of adenylyl cyclase, leading to an increase in cyclic AMP (cAMP). Increased cAMP levels then activate protein kinase A (PKA), which phosphorylates various proteins involved in smooth muscle contraction, ultimately leading to relaxation and bronchodilation.
Clinical Significance of Bronchodilation
The bronchodilatory effect of sympathetic activation is crucial for maintaining normal respiratory function. During periods of increased physical activity or stress, the sympathetic nervous system is activated, leading to bronchodilation, which increases airflow and oxygen uptake, enhancing the body's capacity to meet the increased metabolic demands. This mechanism is also exploited therapeutically. β2-agonists, drugs that selectively stimulate β2-adrenergic receptors, are widely used as bronchodilators in the treatment of asthma and chronic obstructive pulmonary disease (COPD). These medications mimic the effects of sympathetic activation, providing rapid relief from bronchospasm.
Beyond Bronchodilation: Other Effects of Sympathetic Activation in the Lungs
While bronchodilation is the most prominent effect, the impact of sympathetic activation on lung function extends beyond airway caliber.
Modulation of Airway Secretion
Sympathetic activation can influence airway secretion, though the effects are more complex and less consistently observed compared to bronchodilation. Some studies suggest that sympathetic stimulation can inhibit mucus secretion, potentially through the activation of α-adrenergic receptors or other indirect mechanisms. However, the overall impact of sympathetic activation on mucus production remains a subject of ongoing research, with the influence likely varying based on specific lung regions, underlying conditions, and other interacting factors.
Pulmonary Vascular Tone
Sympathetic activation also affects pulmonary vascular tone. While the primary impact on bronchi is relaxation, its effect on blood vessels is more nuanced. Norepinephrine acting on α1-adrenergic receptors on pulmonary vascular smooth muscle can cause vasoconstriction, reducing blood flow through the pulmonary circulation. However, β2-adrenergic receptor stimulation on pulmonary vessels can lead to vasodilation. The overall effect on pulmonary vascular tone depends on the relative activation of these opposing receptor subtypes, as well as other factors such as blood oxygen levels and circulating hormones.
Influence on Lung Immune Cells
Sympathetic nerve activity can modulate the activity of immune cells within the lung tissue. Norepinephrine, acting on adrenergic receptors expressed by various immune cells (e.g., macrophages, lymphocytes), can influence the production of cytokines and other inflammatory mediators. This modulatory effect is complex and can vary depending on the specific cell type, the type of adrenergic receptor involved, and the overall inflammatory context. Studies suggest that sympathetic activation can both enhance and suppress immune responses depending on these various factors, highlighting the intricate interplay between the nervous and immune systems within the lungs.
Interactions with Other Systems
The sympathetic nervous system doesn't operate in isolation. Its effects on the lungs are intricately intertwined with the actions of other systems, including the parasympathetic nervous system (which promotes bronchoconstriction and increased mucus secretion), the endocrine system (hormones such as cortisol can influence adrenergic receptor sensitivity), and the local inflammatory milieu. This interplay of various regulatory mechanisms ensures a finely tuned control of pulmonary function, adapting to diverse physiological states and environmental challenges.
Clinical Implications and Future Directions
Understanding the multifaceted effects of sympathetic activation on lung tissue is crucial for advancing our understanding and treatment of respiratory diseases. As mentioned earlier, β2-agonists effectively mimic the bronchodilatory effects of sympathetic stimulation, playing a pivotal role in the management of asthma and COPD. However, the complexities of sympathetic modulation of airway secretion, vascular tone, and immune responses suggest potential avenues for therapeutic intervention beyond simply targeting bronchodilation.
Future research directions include exploring the potential of:
- Developing novel therapies that selectively target specific adrenergic receptors in the lungs to achieve more precise modulation of airway caliber, mucus secretion, and vascular tone.
- Investigating the role of sympathetic nervous system dysfunction in the pathogenesis and progression of various respiratory diseases, including asthma, COPD, and lung fibrosis.
- Exploring the therapeutic potential of targeting the interactions between the sympathetic nervous system and the immune system to develop novel anti-inflammatory treatments for pulmonary diseases.
Conclusion
Activation of sympathetic nerves innervating lung tissue results in a complex interplay of physiological responses, with bronchodilation being the primary and most prominent effect. However, the influence of sympathetic activation extends beyond simple airway dilation, impacting airway secretion, pulmonary vascular tone, and immune responses within the lung. A thorough understanding of these multifaceted effects is critical for developing improved therapeutic strategies for various respiratory disorders and improving our comprehension of pulmonary physiology as a whole. Ongoing research in this field holds the potential to unlock novel therapeutic targets and innovative approaches to managing and treating lung diseases.
Latest Posts
Latest Posts
-
Which Of The Following Is True Regarding An Acknowledgments Section
Apr 02, 2025
-
Lehninger Principles Of Biochemistry 8th Edition
Apr 02, 2025
-
Label The Cladogram Of Terrestrial Vertebrates
Apr 02, 2025
-
Employees Are Likely To See An Adaptive Change As
Apr 02, 2025
-
Happy Go Lucky Electric Company Is The Only Company
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Activation Of Sympathetic Nerves That Innervate Lung Tissue Results In . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
